-
PDF
- Split View
-
Views
-
Cite
Cite
Yotsapon Thewjitcharoen, Taweesak Srikummoon, Nuchjira Srivajana, Panitta Plianpan, Soontaree Nakasatien, Thep Himathongkam, Hemorrhagic necrosis of small bowel following small bowel obstruction as a late complication of sex reassignment surgery—a gap in transgender care, Journal of Surgical Case Reports, Volume 2018, Issue 11, November 2018, rjy314, https://doi.org/10.1093/jscr/rjy314
Close - Share Icon Share
Abstract
For decades, Thailand has been at the forefront of sex reassignment surgeries. The neovagina created by recto-sigmoid vaginoplasty is much more complex procedure when compared with penile skin version technique, but yielded more satisfactory functional outcomes. We reported an unusual case of life-threatening small bowel obstruction following previously successful recto-sigmoid vaginoplasty in a transgender woman. Transgender individuals have unique healthcare needs. However, various gaps still exist to provide multi-disciplinary care for these patients. The rate of adhesive small bowel obstruction is highest in the early period of any intra-abdominal post-operative surgeries, but the risk remains life-long. Transgender women receiving complicated vaginoplasty should be instructed to continue long-term follow-up to ensure early detection and management of post-operative complications.
INTRODUCTION
Transgender people are individual whose gender identity does not match with their sexual anatomy [1]. For many transgender adults, sex reassignment surgery (SRS) would be the necessary procedure to achieve optimal aesthetic and functional outcomes like the opposite desired gender role [2]. Reconstructive genital surgery that preserves neurologic sensation is the cornerstone procedure in transitioning to the opposite sex [3, 4]. For decades, Thailand has been at the forefront of SRS especially in transgender women (male to female) due to its low-cost and high-quality medical care. However, various gaps still exist to provide multi-disciplinary care for transgender patients. Most transgender people (both local Thai people and foreigners) seek their gender treatments privately in specialized clinics or hospitals which are well-known in their social media communities. From the recent review article regarding the current situation of SRS in Thailand [5], surgery is commonly performed when patients have received unsupervised use of hormone therapy for at least 5 years (usually in their 20s). Apart from the risks arise from inadvertent use of supraphysiologic doses of sex hormones, unregulated surgical treatments or lack of long-term post-operative care could lead to the devastating results in transgender people [6].
Herein, we reported an unusual case of life-threatening small bowel obstruction following previously successful recto-sigmoid vaginoplasty in a transgender woman. This underscores the importance of a thorough personal history and general evaluation of the transgender patient who presented with acute abdominal pain as well as emphasized on perception of post-operative surgical risks remains life-long after SRS.
CASE REPORT
A 28-year-old Thai transgender woman patient presented to the emergency room with acute periumbilical pain and then developed hematochezia with hypovolemic shock at 12 h later after admission. She denied history of recent trauma or sexual intercourse had no hematemesis or melena. Careful history taking revealed that the patient had undergone male to female gender reassignment surgery (surgically removing natal gonads along with recto-sigmoid vaginoplasty) 18 months earlier at another private hospital but patient was lost to follow-up after 1 year. She was successfully living in the female role after operation with occasional symptoms of recurrent abdominal pain for a few times but spontaneously resolved without seeking medical attention.
Physical examination demonstrated marked abdominal distension and tenderness. Abdominal X-ray showed dilated small bowel without free air. Ultrasound-guided paracentesis revealed unclotted blood so the hemoperitoneum was diagnosed and the patient underwent an emergency laparotomy. Exploratory laparotomy revealed 100-cm hemorrhagic necrosis of a segment of jejunum secondary to post-surgical fibrous adhesions (Fig. 1) with ~2000 mL of blood in the abdominal cavity. Segment of necrotic small bowel was removed. There were no masses, ulcers, scarring or perforations in the excised small bowel. Microscopically, transmural vascular congestion and hemorrhagic necrosis were observed in the sections of small bowel with normal lumen of mesenteric arteries (Fig. 2). Post-operatively, the patient remained well without immediate complications.
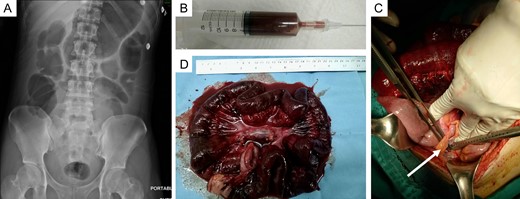
(A) Abdominal X-ray showed dilated small bowel without free air. (B) Ultrasound-guided paracentesis revealed unclotted blood. (C) One hundred-centimeter segment of necrotic jejunum secondary to adhesion band (arrow) was found at the time of exploratory laparotomy. (D) Resected specimen showed diffuse dark discoloration of the ischemic segment of mid-small intestine.
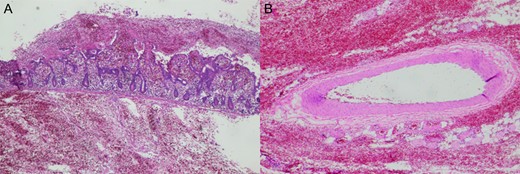
(A) Sections of small bowel showed transmural hemorrhagic necrosis with acute inflammatory exudates and congestion. (B) Mesenteric arteries supplying the segment of excised small bowel contained no thrombi.
DISCUSSION
Transgender issue has gained momentum recently in the media and been increased acceptance by the general public and medical community. While little has changed in terms of hormone regimens, more and more transgender women decide to undergo SRS to have aesthetic and functional external female genitalia [4]. However, surgical intervention represents only one aspect of the treatment which should be provided under multi-disciplinary care for these patients. Previous studies [2, 6] have shown that the majority of transgender individuals do not regularly access proper medical care and also the substantial costs of SRS especially in developed countries restricted the ability of transgender individuals to obtain surgery in their home countries. As a result, Thailand became one of the leading destinations for transgender individuals worldwide to receive SRS.
Many surgical methods for vaginoplasty have been developed in the past decades. Currently, the most common technique is a penile-scrotal skin flap to create the neovaginal vault. However, sometimes there is inadequate tissue to form a full neovagina, so surgeons have revisited using intestine to create neovagina. This technique was first reported by since 1907 in patients with vaginal agenesis but only introduced in the field of transgender medicine for the last 3 decades [7]. The neovagina created by recto-sigmoid vaginoplasty is much more complex procedure when compared with penile skin version technique, but yielded more satisfactory functional outcomes [8].
The recent retrospective analysis on intestinal vaginoplasty found that there was an overall complication rate of 6.4% for the sigmoid neovagina in 686 patients which most complications occurred within 1 year [7].
Severe complications included necrosis of the sigmoid conduit, necrotizing fasciitis, an intra-luminal abscess in the top of the neovagina. Small bowel obstruction developed between 2 months and 2 years after surgery was found in only six cases (0.9%). Based on these limited evidences, intestinal vaginoplasty appears to be a safe procedure with a beneficial outcome. The common practice of private hospitals in Thailand usually follow up Thai patients who receiving vaginoplasty until 1 year after surgery, while foreigner patients are usually receiving their last follow-up with their surgeon 2 weeks after surgery and then they are instructed to continue their care with endocrinologists or gynecologists in their home countries [5]. However, transgender women receiving complicated vaginoplasty should be instructed to continue long-term follow-up to ensure early detection and management of post-operative complications.
In our reported case, the patient was lost to follow-up after 1 year post-operatively and she recalled symptoms of partial gut obstruction which resolved spontaneously before this admission. Operated adhesive post-operative SBO has a high recurrence rate which ranges from 7 to 26% and needs surgical correction from 2.6 to 6.7% at 2–10 years [9]. Outcome of this condition is mainly based on the early diagnosis and intervention. Massive hemoperitoneum in our case was an unexpected finding which could result from hemorrhagic infarction of small bowel and impending perforation of bowel wall. Substantial increases in intra-luminal pressure from a close-loop obstruction might lead to compromise vascular supply to the bowel wall as a previous reported in a fatal case of small bowel volvulus [10].
ACKNOWLEDGEMENTS
The authors gratefully thank the patient who permitted us to publish this case. A written informed consent was obtained for publication of this case report.
CONFLICT OF INTEREST STATEMENT
None declared.



