-
PDF
- Split View
-
Views
-
Cite
Cite
Christer D Johansen, Jan Norum, Bernt E Engebretsen, Uwe Agledahl, A nutrition problem solved by a two-step endoscopic removal of a non-adjustable gastric band, Journal of Surgical Case Reports, Volume 2018, Issue 11, November 2018, rjy306, https://doi.org/10.1093/jscr/rjy306
Close - Share Icon Share
Abstract
Bariatric surgery is an effective approach for weight loss and short-term improvement in metabolic disorders. Stenosis is a common complication of gastric banding. Balloon dilatation or gastrotomy has been employed in this setting. Few studies have indicated endoscopic removal of the band a feasible procedure. We present a 60-year-old female who underwent gastric banding in 1985 and suffered from late stenosis and malnutrition. Endoscopy revealed a severe stenosis. A two-step procedure was performed. Initially a coated stent was placed into the stenosis to achieve pressure necrosis. Two weeks later, the stent was removed and the band was removed endoscopically. The procedure was performed without any complications. The patient was discharged the next day. A follow-up after 2 months revealed no problems with stenosis or malnutrition. The procedure was a safe, efficient and convenient way of handling late stenosis after gastric banding.
INTRODUCTION
Lifestyle and diet patterns have rapidly increased the prevalence of obesity. Bariatric surgery is an effective approach for weight loss and short-term improvement in metabolic disorders. Techniques employed have been Roux-en-Y gastric bypass (RYGB), sleeve gastrectomy (SG) and laparoscopic adjustable gastric banding (LAGB). They are all considered first-line treatment options in patients with severe obesity [1]. However, there are several possibilities of complications as anastomotic leak, bleeding, stricture, marginal ulcers, dilation of gastrojejunal (GJ) anastomosis or gastric pouch, and band erosions [2]. The management of these complications has become important as they can be life-threatening, if not managed promptly [3].
Postoperative stricture or dysfunctioning bands or rings occur in 4–17% of patients [2]. Balloon dilatation may be a successful treatment, but the risk of complications, especially leaks due to perforation is not uncommon [1]. Removal of the ring or band through a gastrotomy may be an alternative [4]. Endoscopic therapy may also be a useful option for a feasible and safe management of complications, such as leaks and stricture/stenosis. The number of studies using the replacement of a stent at the stricture has been very few and the studies have been small [1, 4–7]. In this case report, we illustrate a two-step endoscopic removal of a non-adjustable gastric band.
CASE REPORT
A 60-year-old female, who had undergone gastric banding in 1985, was referred in February 2018 to our institution due to malnutrition and weight loss. Her weight and height were 66 kg and 168 cm, respectively. She had developed increasing malnutrition problems due to a stenosis in the stomach (due to gastric banding) and could not eat regular food. Her food intake was a liquid diet in terms of various soups and nutrition drinks. A blood test relieved normal values of hematology, electrolytes, and kidney and liver functions. A gastroscopy documented a 6 cm long upper part of the ventricle and a two cm long stenosis. An X-ray of esophagus, stomach and duodenum (Fig. 1) revealed a very slow passage through the stenosis. After 15 min the barium agent had passed through the stenosis. The diameter of the stenosis was measured by the radiologist to be 8 mm. There was still barium contrast left in the upper part after 12 h.
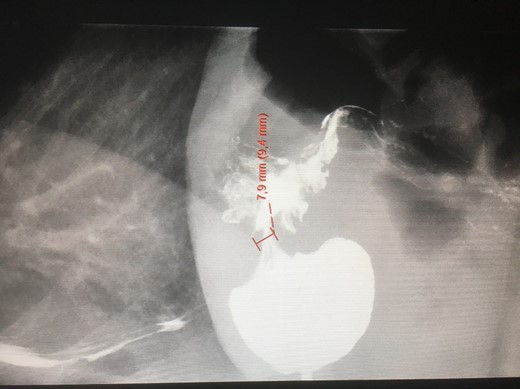
An X-ray of the stomach with gastric banding and a stenosis. Barium has been administered.
The first session after diagnosis was the introduction of a stent. The stent was placed into the stenosis employing an endoscope (Fig. 2a). This to achieve pressure necrosis of the tissue within the stenosis, making access to the gastric band possible. The procedure was performed (according to patient’s wish) in general anesthesia.
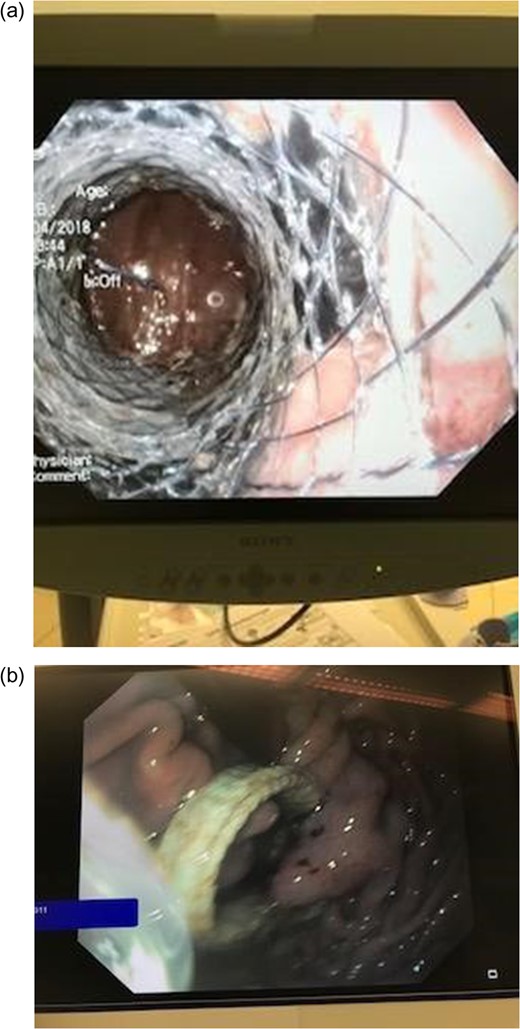
The figure illustrates the inserted stent. (a) The gastric stent in position in the stenosis and (b) the available gastric band due to tissue necrosis.
The next sessions was done 2 weeks later. The stent was endoscopically removed and due to tissue necrosis, the gastric band was now present inside the stomach wall (Fig. 2b). The gastric band was carefully removed by an endoscope. The procedure was performed in general anesthesia and no complications occurred. The patient was requested not to eat during the next 3 h. The day after, she left the hospital. We called her 2 months later. She had no problem with stenosis or malnutrition. She now ate regular food.
DISCUSSION
LAGB is considered a safe and effective method of weight loss and reduction of comorbidities associated with obesity. However, patients undergoing bariatric surgery may deal with postoperative stricture or dysfunctioning bands or rings that should be removed [8]. Postoperative stricture is one of the most frequent complications and the reported incidence has been in the range of 4–17% [1]. Endoscopy may play a pivotal role in the management of this post-bariatric complication. A balloon dilatation has been a frequently employed treatment alternative. However, serious complications, including perforation, have been reported [1]. Campos et al. [9] showed that gastric pouch outlet stenosis due to silastic ring slippage after RYGB was successfully managed with preliminary dilation using a dilator (Cook Biotech Inc.) or a CRE balloon dilated up to 20 mm, followed by definitive dilation using a 30-mm achalasia balloon.
A common alternative is the removal of the ring or band through a gastrotomy done by laparoscopy [4]. However, recently some small studies and case series, using the replacement of a stent at the stricture, has been shown promising [4, 6, 7, 10]. The success rate of endoscopic removal of bands that have been almost intragastrically migrated by the use of tools as endoscopic scissors, laser or gastric banding cutters have been reported ranging between 56 and 100%. Blero et al. [4] reported one failures due to huge adhesions between the connection site of the band with the reservoir lining on the lesser curvature of the stomach and the lower face of the left liver lobe. They concluded that a two-step procedure would have solved the problem. In our case we employed this procedure. Initially, a coated stent was inserted and a pressure necrosis occurred during the following 2 weeks. This approach has also been employed by others [4, 10]. A temporary insertion of fully covered stents for 1–2 weeks induce and accelerate the process of band erosion. This by the induction of pressure necrosis of the gastric wall between the band and stent. During the next session, the stent can be removed and the gastric banding released and removed. The process may be performed with the patient under general or local anesthesia [4, 10].
The endoscopic stent placement can also be employed in treating leaks [1]. This together with the injection of fibrin glue. A novel full-thickness closure over-the-scope clip has also been used for treatment of postoperative leaks.
In our case, the follow-up was taken care of by phone. Based on the experience of Campos et al. [9], a follow up is necessary. They reported that a successful removal of the band was achieved in all patients, but nine patients (22%) required additional endoscopic balloon dilation after removal of the stent.
CONCLUSION
In summary, endoscopic removal of dysfunctioning bands or rings is safe, effective and feasible by the use of a two-step endoscopic procedure.
CONFLICT OF INTEREST STATEMENT
The authors have no conflicts of interests or disclosures.



