-
PDF
- Split View
-
Views
-
Cite
Cite
H Guadalajara Labajo, M León Arellano, J Vaquero Crespo, I Valverde Núñez, D García-Olmo, Objective demonstration of improvement of neurogenic bowel dysfunction in a case of spinal cord injury following stem cell therapy, Journal of Surgical Case Reports, Volume 2018, Issue 11, November 2018, rjy300, https://doi.org/10.1093/jscr/rjy300
Close - Share Icon Share
Abstract
Constipation in spinal cord injury patients is a frequent complication that leads to a reduction of quality of life, extensive psychological and economic strain on patients and healthcare systems. We report a 58-year-old man with an incomplete SCI secondary to L1 vertebral fracture, presented gait disorder with neurogenic bowel and bladder dysfunction. He received 300 million autologous mesenchymal stromal cells (MSC) in the subarachnoid space by lumbar puncture. After the third administration of MSC the patient had an important improvement in almost every functional scale of spinal cord injury, especially in the Krogh's Neurogenic Bowel Dysfunction scale. Our present observation supports recent clinical findings about the benefit of autologous stem cell therapy for the improvement of bowel dysfunction in patients suffering spinal cord injury.
INTRODUCTION
Neurogenic bowel dysfunction includes constipation, abdominal pain and fecal incontinence, this are frequent complications of spinal cord injury (SCI). Severe constipation could be present in more than 30% of this patient. Other complications include neuropathic and musculoskeletal pain, pressure ulcers, problematic spasticity and urinary tract infections.
The patients with SCI have delayed colonic motility and anorectal dysfunction resulting in functional obstruction and constipation. This may be caused by changes in descending modulation from the central or sympathetic nervous systems [1].
Treatment include conservative management when possible, however, surgical procedures such as a colostomy may be indicated. Despite recent advances in the treatment of neurogenic bowel dysfunction, a significant proportion of subjects with SCI continue to have severe symptoms [2].
Neuroregenerative strategies to treat patients with SCI, aim to replace the damaged cells, axons and circuits in the spinal cord, by either modifying the injury environment to stimulate endogenous regeneration or cell transplantation [3]. It has been hypothesized that the therapeutic effect of stem cells may be due to their immunoregulatory and anti-inflammatory properties, which may work together to accelerate healing [4].
Recently, cell therapy with autologous bone marrow mesenchymal stromal cells (MSCs) supported in autologous plasma has been associated to a clear and early improvement in symptoms of neurogenic bowel dysfunction. This finding has been reported when MSCs were transplanted into an injured zone of SCI [5] or after repeated administration of MSCs in subarachnoid space by lumbar puncture [6]. However, in these studies, objective data provided by anorectal explorations were not shown.
In this report, we show by the first time, objective data about the functional anorectal modifications occurred after cell therapy in a patient with SCI.
CASE REPORT
A 58-year-old man with an incomplete SCI (ASIA C and neurological level at Th12) secondary to L1 vertebral fracture (Fig. 1), presented a 32-year history of gait disorder with neurogenic bowel and bladder dysfunction.

The patient had undergone several years of rehabilitation without improvement in his neurological symptoms.
Intermittent bladder catheterization was used for urinary dysfunction and presented a severe constipation with a defecation frequency every week with the need of laxatives and digital evacuation.
Preoperative test
Initial physical examination revealed an atonic anal sphincter and a pelvic floor descent.
An endorectal ultrasound was done, the external anal sphincter showed no lesions and a thin internal sphincter without mobility. Anorectal manometry showed basal resting pressure and anal squeeze pressure of 35–40 mmHg. Also, a hypotonic internal anal sphincter, lack of external anal sphincter contraction and a complete absence of rectal sensibility due to distension despite high volumes. Rectoanal inhibitory reflex was present.
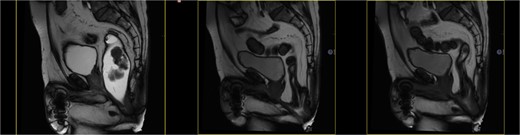
Dynamic MRI: Important rectal prolapse and pelvic floor descent. The evacuation after the introduction of the endorectal contrast was incomplete. (Fig. 2)

In the Krogh´s Neurogenic Bowel Dysfunction scale [7] presented a Severe condition with 19 points.
Previous authorization of the ethic committee and a signed informed consent, the patient was included in a clinical trial to study the effects of cell therapy in patients suffering SCI (EudraCT 2014-005613-24).
Cell therapy medicament
We used a cell therapy medicament (NC1) currently approved as a medicament under clinical investigation by the AEMPS (PEI No. 12–141). It consists of autologous MSCs and autologous plasma as its excipient.
For culture of MSCSs, 50 mL of bone marrow was aspirated under aseptic conditions from the iliac bones and sent to a cleanroom for culture and expansion under good manufacturing practice (GMP). The cultures were maintained at 37°C in a humidified 5% CO2 atmosphere for 3 days, after which non-adherent cells were removed by replacing the medium. When the cultures approached confluence (90–100%), adherent cells were detached by treatment with trypsin/ethylenediamine tetraacetic acid (EDTA) solution (BioWhittaker-Lonza).
Criteria for the administration of MSCs included a viability >95%, absence of microbial contamination (bacteria, fungus, virus or mycoplasma), expression of CD105, CD90, HLA I, CD73 and CD166 for more than 90% of cells, and absence of CD34, CD80, HLA II, CD45 and CD31 (expression of each <5%), as assessed by flow cytometry.
Surgery description
He received 300 million autologous MSCs in the subarachnoid space by lumbar puncture, at a dose of 100 millions every 3 months in the Cell Therapy Unit.
Postoperative test
After the third administration, the patient had an important improvement in almost every functional scale of spinal cord injury, especially in the Krogh´s Neurogenic Bowel Dysfunction scale, at this point with a Minor Bowel Dysfunction grade with 6 points.
Six months after first treatment, an anorectal manometry was done, showing an increased basal resting pressure of 82 mmHg and anal squeeze pressure of 105.4 mmHg. Slight improvement in rectal sensibility. Rectoanal inhibitory reflex was present.
Dynamic MRI: Important rectal prolapse and pelvic descent without changes. The evacuation after the introduction of the endorectal contrast was complete (Fig. 3).
The patient referred less soiling, but defecatory diary is not evaluable due to the regular use of a rectal irrigator device.
DISCUSSION
Constipation in spinal cord injury patients is a frequent complication that leads to a reduction of quality of life, extensive psychological and economic strain on patients and healthcare systems [8].
When conservative treatments fail to improve the constipation, Malone anterograde continence enema and sacral anterior root stimulator implantation, and even more aggressive procedures like colostomy, ileostomy, must be considered [9].
Our present observation supports recent clinical findings about the benefit of autologous stem cell therapy for the improvement of bowel dysfunction in patients suffering SCI [5, 6].
The mechanism of improvement is difficult to establish, but the possibility that MSCs may act through the release of neurotrophic factors has been pointed out [6]. In any case, the improvement in neurogenic bowel dysfunction after cell therapy, at least using autologous bone marrow MSCs supported in autologous plasma is configured as a virtually constant finding [5, 6] that can be objectified not only by the application of functional scales, but also by objective data for anorectal exploration, as we show in our present case (Table 1).
| . | Before treatment . | After treatment . |
|---|---|---|
| Manometry | ||
| Basal resting pressure | 35–40 mmHg | 82 mmHg |
| Anal squeeze pressure | 35–40 mmHg | 105.4 mmHg |
| Rectal sensibility | Absence | Present |
| Rectoanal inhibitory reflex | Present | Present |
| Dynamic MRI | ||
| Contrast evacuation | Incomplete | Complete |
| M-line descent | 9 cm | 9 cm |
| Krogh´s Neurogenic Bowel Dysfunction scale | 19 pts | 6 pts |
| . | Before treatment . | After treatment . |
|---|---|---|
| Manometry | ||
| Basal resting pressure | 35–40 mmHg | 82 mmHg |
| Anal squeeze pressure | 35–40 mmHg | 105.4 mmHg |
| Rectal sensibility | Absence | Present |
| Rectoanal inhibitory reflex | Present | Present |
| Dynamic MRI | ||
| Contrast evacuation | Incomplete | Complete |
| M-line descent | 9 cm | 9 cm |
| Krogh´s Neurogenic Bowel Dysfunction scale | 19 pts | 6 pts |
| . | Before treatment . | After treatment . |
|---|---|---|
| Manometry | ||
| Basal resting pressure | 35–40 mmHg | 82 mmHg |
| Anal squeeze pressure | 35–40 mmHg | 105.4 mmHg |
| Rectal sensibility | Absence | Present |
| Rectoanal inhibitory reflex | Present | Present |
| Dynamic MRI | ||
| Contrast evacuation | Incomplete | Complete |
| M-line descent | 9 cm | 9 cm |
| Krogh´s Neurogenic Bowel Dysfunction scale | 19 pts | 6 pts |
| . | Before treatment . | After treatment . |
|---|---|---|
| Manometry | ||
| Basal resting pressure | 35–40 mmHg | 82 mmHg |
| Anal squeeze pressure | 35–40 mmHg | 105.4 mmHg |
| Rectal sensibility | Absence | Present |
| Rectoanal inhibitory reflex | Present | Present |
| Dynamic MRI | ||
| Contrast evacuation | Incomplete | Complete |
| M-line descent | 9 cm | 9 cm |
| Krogh´s Neurogenic Bowel Dysfunction scale | 19 pts | 6 pts |
In conclusion, the administration of autologous MSCs into subarachnoid space is a simple and safe procedure [6] that should be considered for the treatment of severe constipation in SCI patients.
FUNDING
None.
CONFLICT OF INTEREST STATEMENT
The authors have no commercial, proprietary or financial interest in the products used.



