-
PDF
- Split View
-
Views
-
Cite
Cite
Roseanne Tobin, Niamh Barry, Niamh M Foley, Fiachra Cooke, A giant duodenal diverticulum causing Lemmel syndrome, Journal of Surgical Case Reports, Volume 2018, Issue 10, October 2018, rjy263, https://doi.org/10.1093/jscr/rjy263
Close - Share Icon Share
Abstract
An 80-year-old female, with a known periampullary giant duodenal diverticulum, presented to the emergency department with general deterioration. While not clinically icteric, her laboratory investigations revealed an obstructive jaundice. MRCP demonstrated mild distension of the gallbladder with several calculi. There was intra- and extra-hepatic biliary dilatation to the level of the ampulla. A giant fluid and air filled periampullary duodenal diverticulum measuring ~8 cm in the long axis was noted. The CBD was dilated to the level of this diverticulum and the cause of the patient’s biliary dilatation and obstruction. A rare pancreaticobiliary complication of duodenal diverticula is Lemmel syndrome. Lemmel syndrome is defined as an obstructive jaundice caused by a periampullary duodenal diverticulum compressing the intra-pancreatic portion of the common bile duct with resultant dilatation of the extra- and intra-hepatic bile ducts. Recognition of this condition is important, as delayed diagnosis can result in unnecessary further investigations.
INTRODUCTION
Lemmel syndrome is defined as an obstructive jaundice caused by a periampullary duodenal diverticulum compressing the intra-pancreatic part of the common bile duct with resultant upstream dilatation of the extra- and intra-hepatic bile ducts [1]. Duodenal diverticula are pseudo-diverticula consisting of extraluminal sac-like out-pouchings of the duodenal mucosa which lack a muscularis layer [2]. Periampullary duodenal diverticula (PAD) are those that develop within a 2–3 cm radius from the ampulla of Vater [3]. PAD are mainly asymptomatic but can, in rare circumstances, cause pancreaticobiliary complications when simultaneously inflamed [4]. Rarely, obstructive jaundice can develop secondary to PAD without choledocholithiasis or tumour in the setting of Lemmel syndrome [5]. Here, a case of Lemmel syndrome is presented.
CASE REPORT
An 80-year-old lady presented to the emergency department with a 6-week history of general deterioration. She complained of nausea, reduced appetite, weight loss, weakness and reduced mobility. She denied any vomiting, abdominal pain, melena, haematochezia, haematemesis, fever, chills or altered bowel habit. She had no chest pain, dyspnoea, cough or urinary symptoms. Her past medical history was not relevant. She was a nursing home resident who was largely dependent in activities of daily living.
Her examination was notable for an end colostomy in the left iliac fossa with a reducible para-stomal hernia. There was a grid-iron incision in the right iliac fossa. The remainder of her physical examination was entirely normal, with a Glasgow coma score of 14/15, and no evidence of clinical jaundice. Table 1 outlines the admission and discharge liver function tests.
The remaining laboratory values were unremarkable. An ultrasound of abdomen displayed distension of the gallbladder with a large volume of stones and sludge, as well as intra- and extra-hepatic biliary ductal dilatation.
| . | On discharge . | On admission . |
|---|---|---|
| Bilirubin | 6.4 | 27.4 |
| ALT | 29 | 741 |
| Alkaline phosphatase | 137 | 517 |
| Gamma GT | 110 | 426 |
| . | On discharge . | On admission . |
|---|---|---|
| Bilirubin | 6.4 | 27.4 |
| ALT | 29 | 741 |
| Alkaline phosphatase | 137 | 517 |
| Gamma GT | 110 | 426 |
| . | On discharge . | On admission . |
|---|---|---|
| Bilirubin | 6.4 | 27.4 |
| ALT | 29 | 741 |
| Alkaline phosphatase | 137 | 517 |
| Gamma GT | 110 | 426 |
| . | On discharge . | On admission . |
|---|---|---|
| Bilirubin | 6.4 | 27.4 |
| ALT | 29 | 741 |
| Alkaline phosphatase | 137 | 517 |
| Gamma GT | 110 | 426 |
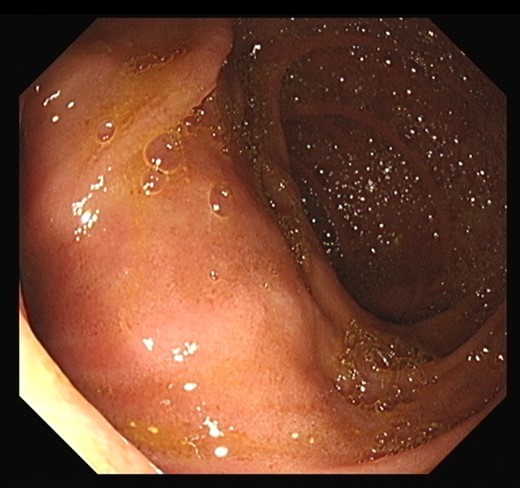
The patient underwent an MRCP which demonstrated mild distension of the gallbladder with several calculi. There was intra- and extra-hepatic biliary dilatation to the level of the ampulla. A very large fluid and air filled periampullary duodenal diverticulum measuring ~8 cm in the long axis was also noted (Figs 1–3). This finding was unchanged compared to a CT study from 6 months previously. The CBD was dilated to the level of this diverticulum and the cause of the patient’s biliary dilatation and obstruction. Interestingly, an unusual appearance to the kidneys was recorded with multiple microcystic changes in both kidneys, which is typically reported in patients with lithium induced renal disease. A gastroduodenoscopy revealed a large periduodenal diverticulum in D2 (Fig. 4).
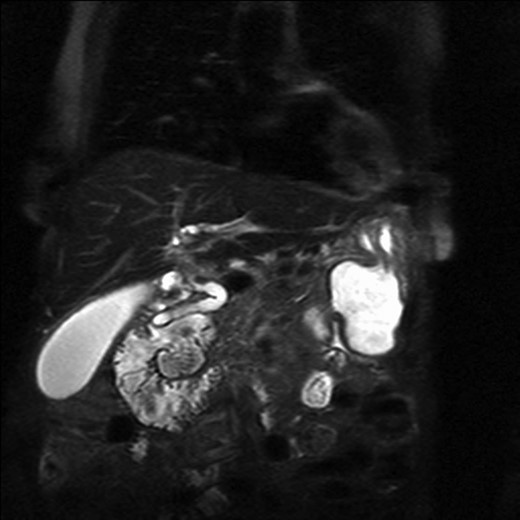
Magnetic resonance imaging with a giant duodenal diverticulum.
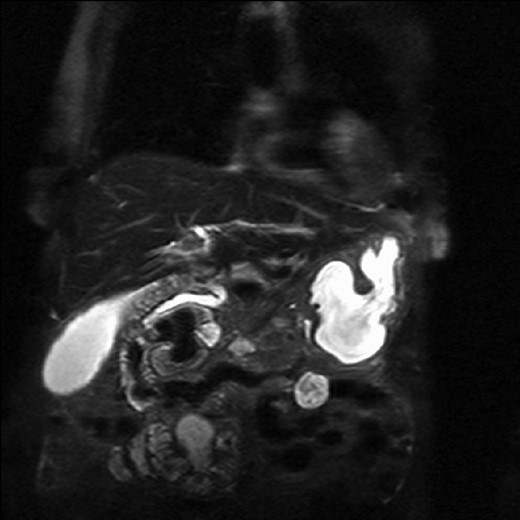
Magnetic resonance imaging with a giant duodenal diverticulum.
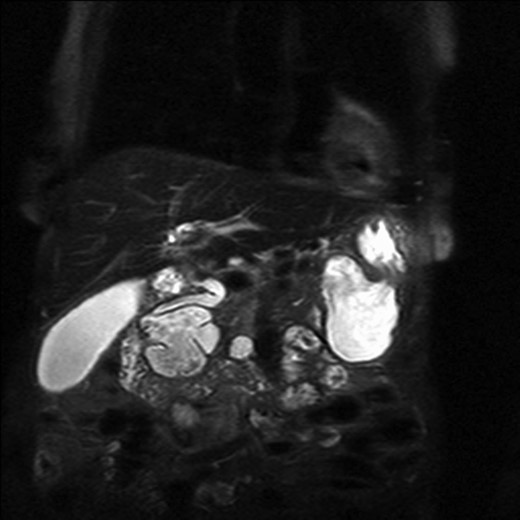
Magnetic resonance imaging with a giant duodenal diverticulum.
DISCUSSION
Diverticula are sac-like protrusions of all or part of the bowel wall that can occur anywhere along the gastrointestinal tract [1]. The most common site for diverticula is the colon, followed by the duodenum [6]. Duodenal diverticula have been reported in 2–5% of patients undergoing barium studies of the upper gastrointestinal tract and in 7% of patients undergoing endoscopic retrograde cholangiopancreatography (ERCP) [7]. Duodenal diverticula most commonly occur within 3 cm of the ampulla of Vater, and these diverticula are termed periampullary diverticula (PAD) [8]. Most of these periampullary diverticuli remain asymptomatic and are diagnosed incidentally, but rarely can cause pancreaticobiliary or non-pancreaticobiliary complications. Non-pancreaticobiliary complications include haemorrhage, diverticulitis, perforation or fistula formation. Pancreaticobiliary complications can include recurrent gallbladder or bile duct stones, obstructive jaundice, acute pancreatitis or ascending cholangitis [9].
Lemmel syndrome was first described in 1934 by Lemmel as obstructive jaundice in the absence of gallstones due to a periampullary duodenal diverticulum [1]. Imaging such as CT scan, MRCP and barium studies are very important in diagnosing this condition. On CT scan and MRCP, PAD may appear as thin-walled cavitary lesions on the wall of the second portion of the duodenum. Barium studies show PAD with contrast-filled out-pouchings that arise from the wall of the descending duodenum [1].
Preferred treatment includes ERCP with sphincterotomy and biliary stent placement—associated with a reduced risk of morbidity and mortality [10]. Other surgical options would include diverticulectomy or bilodigestive anastomosis.
Lemmel syndrome is a rare condition that must be considered as a differential in cases of obstructive jaundice with no choledocholithiasis or tumour. Ignoring the possibility of same can lead to repetitive jaundice and possible cholangitis, increasing the mortality and morbidity risk for the patient.
CONFLICT OF INTEREST STATEMENT
None declared.



