-
PDF
- Split View
-
Views
-
Cite
Cite
Shahab Rafieian, Mehrnaz Asadi Gharabaghi, Tracheopleural fistula after thoracoscopic esophagectomy: novel therapeutic approach with pericardial and intercostal muscle flaps, Journal of Surgical Case Reports, Volume 2018, Issue 10, October 2018, rjy277, https://doi.org/10.1093/jscr/rjy277
Close - Share Icon Share
Abstract
Tracheal rupture following thoracoscopic esophagectomy is a dangerous event requiring primary repair with flap reinforcement. If the injury is not diagnosed during the surgery, morbidity and mortality increase significantly. Meanwhile, primary repair in such cases is not feasible due to the inflammation and difficulty in approximating the defect. Here, we report a case of tracheal injury during thoracoscopic esophagectomy with primary repair failure. We successfully repaired the injury by covering the defect first by a pericardial flap, then reinforcing it with an intercostal muscle flap. To our knowledge, there are few reports of such novel surgical techniques.
INTRODUCTION
Tracheal injuries can occur following esophageal resections in a variety of malignant and benign esophageal diseases. If injuries are diagnosed during the operation with a loss in the airway pressure during ventilation and visible or audible air leak, it must be repaired immediately with primary repair and reinforcement of the suture line with pericardial or intercostal muscle flaps. If not diagnosed early, the injury may lead to increased morbidity and mortality. Small injuries in the thoracic trachea, which are not diagnosed during operation, could cause a lung collapse, empyema and air leak through tracheostomy tube. The delayed diagnosis and failure of primary repairs are rarely reported in the medical literature. Therefore, the treatment has not been exactly defined. Treatment may include a wide spectrum of options, extending from conservative management to surgical intervention. Patients with fully expanded lungs and mild air-leak trough thoracostomy tubes (TT) and no evidence of empyema, or mediastinitiscan have to be managed conservatively. Yet, the presence of the more severe symptoms includes lung collapse, severe air-leak, respiratory complaints and empyema/mediastinitis, necessitating surgical intervention [1–3].
Here, we report a case of tracheal injury following thoracoscopic esophageal resection which was primarily repaired unsuccessfully with no flap reinforcement. The patient suffered right lung collapse and severe air leak thorough tracheostomy tube several days after surgery. We successfully repaired the injury with just a pericardial and intercostal muscle flaps since the primary repair was not feasible due to localized mediastinitis. To our knowledge, it is the first report of such a surgical intervention in repairing trachea injuries.
CASE REPORT
A 66-year-old male patient with esophageal cancer has undergone a thoracoscopic esophageal resection. He was a known case of stage IIb and with a history of neoadjuant chemoradiotherapy. During the thoracoscopic esophageal resection, the posterior membranous wall of the trachea was injured 1 cm above the carina. A cancer surgeon repaired the laceration primarily with a single interrupted suture with no flap reinforcement. He did not convert to thoracotomy. The patient suffered a right lung collapse and a severe air leak from TT on the fifth post-operative day. In consultation with a thoracic surgeon, video bronchoscopy was performed. The patient sustained tracheal injury in the range of 5 × 5 ml 1 cm above the carina, showing the failure of primary repair. Owing to the lung collapse and severe air leak, he was a definite candidate for reoperation.
Under general anesthesia with double-lumen endotracheal intubation, operative repair was done with a right postero-lateral thoracotomy through the fifth intercostal space. At first, the intercostal flap was prepared, whereupon the gastric flap was retracted to expose tracheal laceration. Tracheopleural fistula was seen on the posterior wall of trachea 1 cm above the carina (Fig. 1). Because of the severe inflammation, primary repair was not possible. Therefore, we had to repair the tear with flaps. First, the tear was covered with a rotated pericardial flap and was sutured into the laceration edge with interrupted Vicryl (4.0) (Fig. 2). Then the pericardial flap was reinforced with the intercostal muscle flap (Video). Care was taken not to puncture the endotracheal tube. Finally, the gastric flap was reverted and sutured to surrounding tissue. Two TT were inserted into the ipsilateral thoracic cavity both anteriorly and posteriorly.
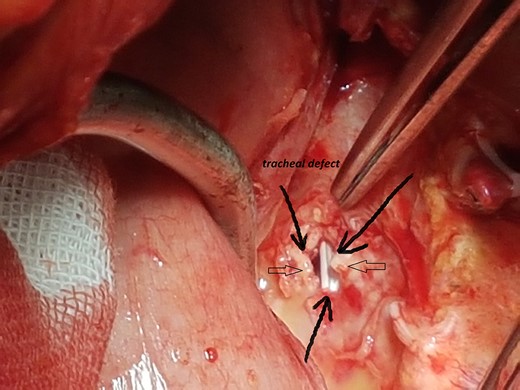
Intra-operative image showing posterior wall defect (open arrows).
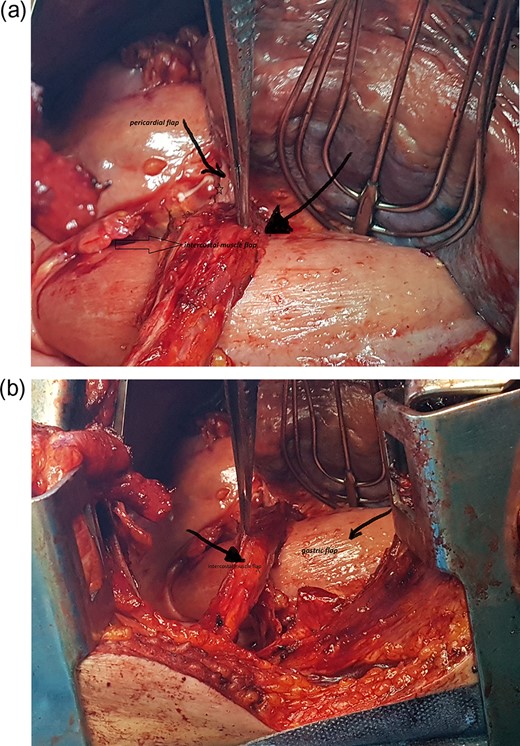
(a and b) Intercostal muscle flap (open arrow) and pericardial flap (star).
He passed the post-operative period in the intensive care unit uneventfully. The air leak stopped on the fifth post-operative day. Video bronchoscopy on the sixth post-operative day showed near completion of the repair of the injury. The day after bronchoscopy the tubes were removed. The patient was discharged 24 h later and followed on out patient base.
DISCUSSION
Tracheal injuries occur in 1–10% of esophagectomies. Previous history of esophageal cancer, preoperative chemoradiation, extensive lymph node mediastinal dissection, peri-tumoral infection and closed proximity of esophageal tumor to carina are the most common predisposing factors [1]. Therefore, transhiatal esophagectomy for proximal tumors must be performed with caution after neoadjuant chemoradiotherapy [1]. When it is recognized during the surgery, tracheal injury must be repaired immediately. However, the management is challenging; the surgical approach depends upon the location of the injury.
In the case of proximal injury, cervical approach with or without partial sternotomy has to be done. Injuries at or above level of carina must be repaired with right postero-lateral thoracotomy after insertion of the double-lumen endotracheal tube. The primary repair of airway injury must be done with interrupted sutures and flap reinforcement. George et al.[1] reported optimal outcome even without flap. All the repairs were carried out during thoracotomy. In our patient, the cancer surgeon did not revert to thoracotomy and sutured the injury with no flap reinforcement. The primary repair without reinforcement and no conversion to thoracotomy might justify the failure of the management and inconsistency of the report by Baht et al. Uwatoko et al. reported tracheal injury during thoracoscopic esophagectomy in a patient with advanced cancer. They converted to minithoracotomy and repaired the injury with a primary sutured and reinforcement with gastric tube [4]. It seems once the injury is identified during thoracoscopy, minithoracotomy is the preferred approach to repair because the use of pediculated muscle flap is not possible with thoracoscopy. Pericardial flaps are not safe enough for the coverage of tracheal laceration due to poor vascularization and paradoxical movement especially under positive pressure ventilation [5]. Therefore, the reinforcement of pericardial flap with an intercostal muscle flap might increase the success of procedure.
In our technique, we have covered the defect with transposed pericardial flap and reinforced it with an intercostal muscle flap. There are successful reports of the primary repair with a pericardial reinforcement. Yet, the hypovascular nature of pericardium has been always a major concern [1]. Therefore, we buttressed the pericardial patch with intercostal muscle flap to avoid any failure. The ease of access and availability prompted us to use intercostal muscle flap. Lung expansion, and air leak stoppage on the fifth post-operative day, and bronchoscopy exam all demonstrated the success of this technique.
CONCLUSION
In conclusion, a tracheal injury during esophagectomy must be repaired immediately with a flap reinforcement. The preparation of the muscle flap is not feasible during thoracoscopic esophagectomy; it seems to be a reasonable option to convert to thoracotomy in case of tracheal injury. However, this issue must be addressed in further studies.
CONFLICT OF INTEREST STATEMENT
None declared.



