-
PDF
- Split View
-
Views
-
Cite
Cite
Umesh Jayarajah, Kasun Bandara Herath, Manoj Hilary Fernando, Vipula Chandu de Silva, Serozsha Goonewardena, Testicular adrenal rest tumour in an adult patient with congenital adrenal hyperplasia: a case report and review of literature, Journal of Surgical Case Reports, Volume 2018, Issue 10, October 2018, rjy255, https://doi.org/10.1093/jscr/rjy255
Close - Share Icon Share
Abstract
Late presentations of testicular adrenal rest tumours (TART) are rarely seen in males with congenital adrenal hyperplasia, and are often misdiagnosed as primary testicular germ cell tumours. We report a case of bilateral TART in an adult patient with congenital adrenal hyperplasia who had defaulted treatment. He presented with a gradually increasing swelling of the left testis and genital examination revealed a large hard indurated swelling of both epididymes more prominent on the left side. As imaging was inconclusive, a biopsy was performed which showed features in favour of TART rather than Leydig cell neoplasm and he had good response to steroids. Histopathological evaluation is helpful in cases where there is a strong need for excluding a malignancy. Optimal steroid replacement is the treatment of choice and leads to regression of the lesion in the majority.
INTRODUCTION
Testicular lesions in the background of congenital adrenal hyperplasia (CAH) were first described by Wilkins et al. [1]. These are commonly known as testicular tumours of the adrenogenital syndrome or testicular adrenal rest tumours (TART). It is postulated that TART arise from aberrant adrenal cells which descend with the testes during embryogenesis. Most TARTs are small and clinically undetectable but can rarely present as a clinically palpable mass [2].
Testicular enlargement in CAH can be diagnostically challenging both clinically and histopathologically [2]. They are almost always benign, however, due to their presentation as a mass lesion, tissue biopsy may be needed to exclude a malignancy. Leydig cell tumours and Leydig cell hyperplasia are possible differential diagnoses and distinction is mandatory as the prognosis and treatment greatly differ [2]. We report a case of bilateral TART in an adult patient with CAH which responded to steroid therapy.
CASE PRESENTATION
A 20-year-old male presented with a gradually increasing swelling of the left testis for 1 year duration. He was otherwise asymptomatic. He was diagnosed to have CAH at the age of 1 year but had defaulted treatment at the age of 4 years. The patient had a strong reluctance to seek medical care due to his poor socioeconomic status and fear of receiving an unfavourable prognosis. Genital examination revealed a large hard indurated swelling of both epididymes more prominent on the left side. Left testis was ill-defined with an approximate diameter of 3.5 cm. Ultrasonography showed bilateral enlargement of the testes and epididymes (right testis measuring 41 ml in volume (6.6 cm × 3.7 cm × 2.3 cm), left testis measuring 52.1 ml in volume (6.2 cm × 4.5 cm × 3.6 cm)). In addition, there were bilateral grade-II varicocele. Seminal fluid analysis showed azoospermia.
A biopsy of the right epididymis was performed. The sections revealed nodules of cells with intervening dense fibrous septae. The nodules comprised nests and cords of polygonal Leydig cells with abundant eosinophilic cytoplasm, uniform round nuclei and small nucleoli. Cell borders were distinct and a lymphoid infiltrate was present in the stroma (Fig. 1). Testicular tissue comprised of seminiferous tubules with thickened basement membranes. Residual testicular tissue showed predominantly germ cell aplasia with occasional tubules containing spermatogonia. Most seminiferous tubules contained only Sertoli cells. Spermatocytes, spermatids and spermatozoa were absent. Collections of Leydig cells were noted between the seminiferous tubules. Intratubular germ cell neoplasia or malignancy was absent (Fig. 2).
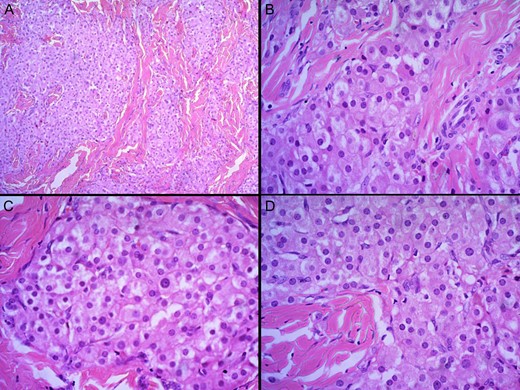
H and E staining viewed under ×4 (A) and ×40 (B–D) showing nodules of cells with intervening dense fibrous septae. The nodules comprised nests and cords of polygonal Leydig cells with abundant eosinophilic cytoplasm, uniform round nuclei and small nucleoli. Cell borders were distinct and a lymphoid infiltrate was present in the stroma.
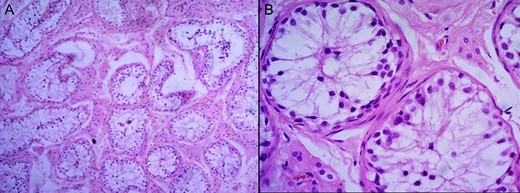
H and E staining viewed under ×4 (A) and ×40 (B) showing testicular tissue comprised of seminiferous tubules with thickened basement membranes. Residual testicular tissue showed predominantly germ cell aplasia with an occasional tubule containing spermatogonia.
Special stains with Mason trichrome did not show Reinke crystals. The cells displayed diffuse cytoplasmic positivity for synaptophysin (Fig. 3). Thus, the histopathological analysis was more in favour of TART rather than Leydig cell neoplasm.
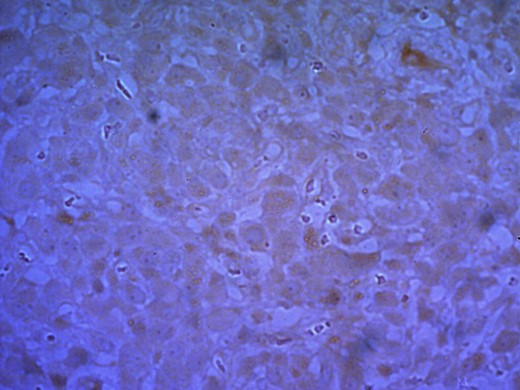
Staining with synaptophysin under ×40 showing diffuse cytoplasmic positivity.
A course of prednisolone was started and there was good response. In 6 weeks, there was marked reduction in the sizes of testes with minimal induration. He was followed up for 6 months but was eventually lost to follow up.
DISCUSSION
Ectopic adrenal rest tissue is found in up to 50% of normal neonates which are found in the retroperitoneum, ovaries, inguinal region, broad ligament and testes [3]. Normally, this ectopic tissue becomes atrophic during development, and persists in <1% of individuals. In patients with CAH, however, the TART occur due to adrenal hyperplasia by the excess stimulation of ACTH [4]. In the majority, the diagnosis of CAH is established before detection of the possible TART. However, due to the wide spectrum of the type and severity of the condition, the clinical presentation differs. Rarely, milder forms of the disease may not be established till early adulthood [3].
Although TARTs are benign, they can be misdiagnosed as Leydig cell tumours. Rarely, in milder forms, the testicular lesion may be the first presentation without a previous diagnosis of CAH [5]. Sometimes, in patients with previous diagnosis of CAH, the testicular lesion may be resistant to treatment which increases the suspicion of a malignancy leading to unnecessary surgery and morbidity.
Histopathologically, TARTs are similar to adrenocortical tissue [6]. They appear as large polygonal cells with abundant eosinophilic cytoplasm arranged in strands or cords separated by fibrous septae. Certain features may help to differentiate TART from Leydig cell tumours. Features such as lack of cytological atypia, low mitotic activity, dense fibrous septa, lymphoid aggregates, adipose metaplasia and prominent lipochrome pigment are more in favour of TART. Reinke crystals are confirmatory of Leydig cell tumours, but is found only in 25–40%. Reinke crystals are absent in TART. Immunohistochemically, diffuse and strong positivity for CD56, negative reactivity for the androgen receptor and focal or diffuse strong reactivity for synaptophysin are noted in TART. On the contrary, weak or negative reactivity for CD56, positive reactivity for the androgen receptor and focal weak or negative reactivity for synaptophysin are demonstrated in Leydig cell tumours [2, 7].
TART are often bilateral while Leydig cell tumours are unilateral. However, association of Leydig cell tumours and CAH have been reported in literature which are mostly unilateral [8]. Furthermore, bilateral Leydig cell tumours and coexistance of TART and Leydig cell tumours in patients with CAH were also reported in literature [9, 10].
In this case report, the presence of bilateral disease with lack of cytological atypia, low mitotic activity, dense fibrous septae and lymphoid aggregates in histological analysis and diffuse reactivity for synaptophysin in immunohistochemical analysis were in favour of TART. CD56 was not available in our facility. He was then given a trial of steroids and there was marked reduction in the size of both testes. Thus clinicians should be aware of late presentation of TARTs in males with CAH to avoid misdiagnosis.
CONCLUSION
In this case, a 20-year-old young patient presented with bilateral synchronous hard testicular lesions in the background of CAH. Late presentations of TARTs are rarely seen in males with CAH, and are often misdiagnosed as primary testicular germ cell tumours or other more common benign testicular lesions. Histopathological evaluation is helpful in cases where there is a strong need for excluding a malignancy. Optimal steroid replacement is the treatment of choice and leads to regression of the lesion in the majority.
ACKNOWLEDGEMENTS
None.
CONFLICT OF INTEREST STATEMENT
The authors declare that there is no conflict of interest.
FINANCIAL SUPPORT
None.
CONSENT
Informed written consent was obtained from the patient for publication.
AUTHORS’ CONTRIBUTION
Authors U.J., K.B.H. and M.H.F. contributed to collection of information and writing of the article. Authors V.C.S. and S.G. contributed to writing and final approval of the article.



