-
PDF
- Split View
-
Views
-
Cite
Cite
Yuliardy Limengka, Wifanto S Jeo, Spontaneous closure of multiple enterocutaneous fistula due to abdominal tuberculosis using negative pressure wound therapy: a case report, Journal of Surgical Case Reports, Volume 2018, Issue 1, January 2018, rjy001, https://doi.org/10.1093/jscr/rjy001
Close - Share Icon Share
Abstract
Enterocutaneous fistula (ECF) is one of the most challenging abdominal complications, for surgeons and other healthcare members, which involves significant morbidity and potentially mortality. Despite advancements in both operative and non-operative therapy, fistula-related complications are still unavoidable. Negative pressure wound therapy (NPWT) had been used years to treat chronic wound, to decrease tissue edema, improve circulation, promote healthy granulation tissue and inhibit bacterial growth. We report a 29-year-old male with complicated ECF due to abdominal tuberculosis, that was healed after treated using NPWT. This was the first ECF patient in our hospital treated using NPWT.
INTRODUCTION
Enterocutaneous fistula (ECF) is considered to be one of the most devastating abdominal complications. Despite being uncommon and not well studied, ECF is associated with considerable morbidity. It can arise as a complication of injury from intra-abdominal surgery, malignancy, inflammatory bowel disease, postradiation therapy for malignancy or as a result of distal obstruction [1]. A mnemonic normally used is FRIEND (foreign body, radiation, inflammation/infection, epithelization, neoplasm and distal obstruction).
The treatment of ECF consists of wound care, nutritional support, infection control, and fluid and electrolyte replenishment [2]. Spontaneous closure of ECF may occur, however, the reported rates are low. In a study of over 250 patients with ECF, it was reported that the spontaneous closure rate and the mortality rates were 50 and 11%, respectively [3]. For numerous patients, non-operative treatments fail, and despite recent surgical advances and improvements, surgery still has a significant morbidity, reported as high as 90%, and carries risks for mortality, between 5 and 21%, although mortality rates below 10% are uncommon [4].
Negative pressure wound therapy (NPWT) has been used for years to treat chronic wounds. The expected results are decreased tissue edema, improved circulation, healthy granulation tissue promotion, and bacterial growth inhibition [5]. Patients may get benefit from higher chance of being healed, reduced length of stay, and reduced fistula-related complications. One of the first studies regarding the use of NPWT in ECF revealed a closure rate of 99% [6], with more recent data reporting closure rates ranging from 26.6 to 81.9%, depending on the type of the NPWT used and the circumstances of the patient [7]. We present a 29-year-old male with ECF due to intestinal tuberculosis treated using NPWT.
CASE REPORT
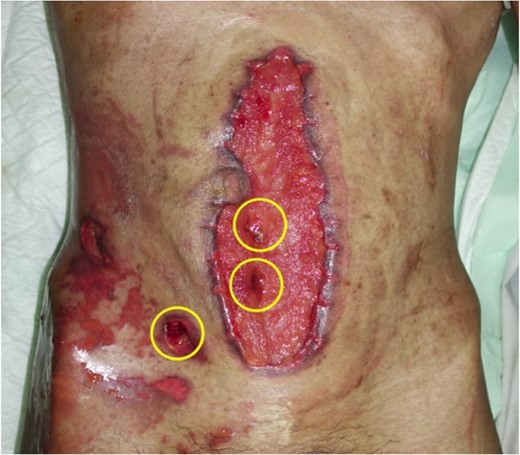
A 29-year-old male presented with abdominal pain and high grade fever. A diagnosis of septic shock and generalized peritonitis was made. Fluid resuscitation was performed and vasopressin was administered, followed by laparotomy. Intraoperatively, severe adhesions were found, with multiple tubercles covering peritoneal wall and intestinal serosa. Rinsing of the peritoneal cavity, tube ileostomy at the perforated intestine, and drain placement were performed. Oral antituberculosis therapy was initiated postoperatively. On postoperative Day 15, intestinal contents were excreted through the laparotomy wound and postdrain wound, as shown in Fig. 1. The patient had developed multiple ECF with a total output of 1500 mL/24 h (Fig. 1).

Wound dehiscence and deep surgical site infection after laparotomy, with multiple fistulas at the surgical site and at the old drainage wound (colostomy bag). The catheter placed is a tube ileostomy.
After unsatisfactory results using conservative wound care for 31 days, as shown in Fig. 2, NPWT was used on the fistulas and the wound surrounding the fistulas, using intermittent pressure of −70 mmHg (5 min of negative pressure and 2 min of rest). Local debridement was performed and new granufoam was reapplied on the wound surface once every 3 days (Figs 2 and 3).

One month after conservative treatment without NPWT. The active high output fistulas are pointed with yellow circles.

After first application of NPWT. White foam was applied on wound surfaces with fistulas, and covered using a black granufoam. The remaining wound surfaces without fistulas were covered using black granufoam alone.
One week after treated using NPWT, the output had decreased to 500 mL/24 h. Productions from the fistulas were able to be controlled as not to spill to the peri-fistula wound. Two weeks post NPWT treatment, the productions had decreased to 70 mL/24 h, and ECF production could easily be controlled to spil into a regular stoma bag. One month following the end of NPWT treatment, healthy granulation tissue had been promoted, and only one active low output fistula left. Keystone flap was performed to facilitate closure. No complications occurred (Figs 4–7).
Wound condition after 1 week treated using NPWT, with three low fistulas remaining, as indicated using yellow circles.

Wound condition after 1 month treated using NPWT, with one low fistula remaining. Healthy granulation tissue indicates the wound is ready for closure.

Wound condition after closure using Keystone flap, with window around one active low output fistula.

One month after closure using flap. Wound contracted, with no active fistula.
DISCUSSION
The management of ECF is challenging, and is associated with high morbidity and mortality. In 1960, NPWT is most frequently applied to chronic wound, as it accelerates the healing process and bring the wound margins closer. The events that underlie the improvement can be classified into primary mechanisms, and their associated secondary effects. Four primary mechanisms of action that have been proposed include wound shrinkage or macrodeformation, microdeformation at the foam-wound surface interface, fluid removal and stabilization of the wound environment. Secondary effects involves the mechanotransduction pathways which alter the biology of wound healing, including angiogenesis, neurogenesis, granulation tissue formation, cellular proliferation, differentiation and migration [8].
We observed that the multiple ECF were obliterated clinically, even with full enteral feeding. The mechanism in which the ECF closure was achieved, is vaguely known, since a pathologic examination was needed to see this on a micro level. One proposed theory is that the stromal tissue which developed during the granulation period, fills the gap, like in chronic wound, and slowly reduces the gap area until fully closed. Another possible explanation, is that the ECFs did not form a direct track, but rather as a result if intra-abdominal spillage that was localized through intestinal adhesion, and finds its way out through another site, and that these spaces gradually obliterated until adhesion closes the perforated bowel.
Previous studies have suggested additional benefits related to the use of NPWT in patients with ECF, including the ability to contain the effluent, protect the skin around the fistula and to prevent further tissue breakdown and improve dermatitis. A previous study reported that wound was noted to be clean, dry and granulating 7–15 days after the start of NPWT [9].
One important factor that delays wound healing is infection. This patient had tuberculous infection, which decreases the host’s ability to fight infection. Inflammation is a normal part of the wound-healing process, and is essential to contaminating micro-organisms elimination. However, in the absence of effective decontamination, inflammation may be prolonged due to incomplete microbial clearance. Both bacteria and endotoxins can lead to prolonged elevation of pro-inflammatory cytokines, which include including interleukin-1 (IL-1) and TNF-α. These may prolong the inflammation phase, and prevent the wound from truly entering remodeling phase. This results in a chronic wound which fails to heal. One of the most popular research interest had been about the elevated level of matrix metalloproteases in chronic wound. Together with the increased protease content, the level of naturally occurring protease inhibitor is decreased. This shift in protease balance may lead to rapid degradation of growth factors in chronic wounds [10].
CONCLUSION
The use of NPWT is useful to patients with ECF both as a definitive or a bridge treatment. It should be considered for all ECF patients that failed conservative treatment. Further prospective studies to analyze the exact role of NPWT in treating ECF are required to identify patients that may get the most benefit.
CONFLICT OF INTEREST STATEMENT
None declared.



