-
PDF
- Split View
-
Views
-
Cite
Cite
Ben Gabbott, Giles Faria, George Lawson, Karen Daly, A Brodie’s abscess with soft tissue collection—complicating an already difficult diagnosis, Journal of Surgical Case Reports, Volume 2018, Issue 1, January 2018, rjx263, https://doi.org/10.1093/jscr/rjx263
Close - Share Icon Share
Abstract
A healthy 14-year-old boy with a 3-month history of thigh pain and swelling is referred to a specialist centre with an uncertain diagnosis. After extensive tests and imaging a Brodie’s abscess is diagnosed. The abscess is complicated by a fistula (cloaca) through the cortical bone of the femur, resulting in a large complex soft tissue collection. This is a presentation, we are unaware has been documented in any literature. After specialist multi-team combined management (Paediatric Trauma and Orthopaedic and Paediatric Infectious Diseases), the patient undergoes two surgical procedures, and extensive antibiotic cover. The patient makes a good recovery with no long lasting sequelae to date.
INTRODUCTION
Brodie’s abscess, a type of subacute osteomyelitis, remains difficult to diagnose due to vague symptoms, insidious onset and lack of systemic reaction. More sinister differentials include malignancy and therefore prompt diagnosis and management of these cases is vital [1]. We present a referral of a 14-year-old male to St Georges Hospital with markedly different symptoms. This article intends to document a very unusual presentation of a Brodie’s abscess.
CASE REPORT
A 14-year-old boy presented with a 3-month vague history of knee and lower thigh pain with swelling of the distal thigh. There was no history of significant trauma. There were no systemic symptoms. His condition deteriorated forcing him to his local A + E, unable to weight bear. Examination revealed a markedly swollen tender right thigh, and reduction in range of movement of the knee. There were no skin changes. Examination of all other joints was normal. The patient was afebrile with normal observations. Blood tests on admission showed a mildly elevated CRP (44 mg/l) and ESR (55), and a normal WBC (9.8 × 10^9/l).
An X-ray, magnetic resonance imaging (MRI) and ultrasound scan was conducted (Fig 1, 2).

Radiograph on presentation to A + E. The radiograph displays ‘a well corticated lesion (15 mm × 17 mm) in the distal femur’.

MRI Images on admission to Hospital. MRI images displaying ‘osteomyelitis with sequestration and erosion through the posterior cortex, extensively extending into the surrounding soft tissues’.
‘A large complex loculated abscess, 10 cm × 8 × 8 cm, extending between the muscles and extended to the posterolateral aspect of the distal femur. A cloaca is present in the cortical bone on the posterior aspect of the distal femur.’
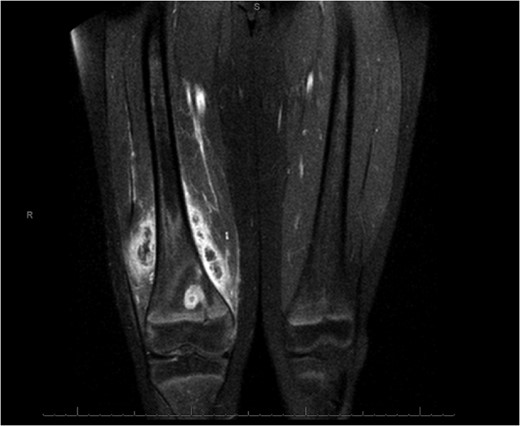
Coronal slice images of presenting MRI, displaying the brodie's abscess and collection.
The working diagnosis was a chronic intraosseous abscess discharging into an extensive soft tissue collection. However, the lack of bone marrow oedema and osteoblastic activity around the rim of the abscess was deemed very unusual by multiple specialists. Advice was sought from the Paediatric Infectious Diseases team, who extensively investigated for immunodeficiency and atypical infections. All of this testing came back negative and the only result of note was a persistently moderately raised CRP and ESR.
After discussion, the patient was taken for surgical drainage. A medial incision was made into the distal thigh over the most fluctuant area, and the tissues, which was visibly filled with purulent fluid, were dissected down to the periosteum. The plane was developed posteriorly to identify the cloaca. Approximately 300 ml of malodorous pus was drained, before a 2- l saline washout was performed. The cloaca was thoroughly curetted, before closure of the skin. Multiple pus samples and swabs were sent for microbiological analysis. The soft tissues and muscles looked well perfused and vital. The tissues were closed and the immediate post-operative period was unremarkable.
Intravenous (IV) ceftriaxone was commenced post-operatively and continued after cultures grew sensitive Staphyloccoccus aureus. At Day 4 post-operatively, the patient reported recurrence of pain in his thigh and he spiked a temperature. Examination revealed a clean, healing medial wound site. However, examination of the lateral side of the patient’s leg revealed localized swelling posterolaterally which had not been present pre-operatively. A repeat ultrasound scan confirmed a persisting collection. With no signs of improvement and with worsening observations and pain, further surgical intervention was indicated.
Surgical drainage was done using a lateral incision. Approximately 150 ml of purulent blood stained fluid was drained from the patient’s leg. Further washout and sample collection were conducted. The wound was not fully closed, and an area ~2 cm was left open, in which a gauze wick was placed to allow for further drainage. The wick was changed using an aseptic technique on a daily basis. The post-operative antibiotic regime chosen was IV Flucloxacillin plus oral Rifampicin (switching to IV Clindamycin). The patient remained on this combination for 5 days. He clinically improved; the collection reduced in size and became less tender, no further temperature spikes were recorded.
The patient was stepped down to IV Flucloxacillin alone, and discharged on this treatment regimen, with regular ward attendance for antibiotics and clinical assessment. He was further stepped down to oral clindamycin and discharged to his local outpatient osteomyelitis clinic. The Orthopaedic team saw him at 6 months after discharge with plain radiographs. The appearance of the radiograph showed satisfactory resolution and he was reverted to 1-year follow-up. There have been no concerns regarding growth and he will be seen once more in a year’s time.
DISCUSSION
Brodie’s abscess, was first described in the literature in 1832 by Sir Benjamin Brodie, as a localized bone abscess that developed without prior systemic illness [2]. Diagnosis of a Brodie’s abscess in a painful limb and absence of systemic symptoms still posses a problematic diagnosis. Furthermore, confirmation of the diagnosis in clinical practice is rare. However, antibiotics are often started without microbiological confirmation [3].
This case was unusual for a Brodie’s Abscess due to the marked soft tissue swelling. Paediatric swellings or lumps are not uncommon. If symptomatic, causing pain and erythema, this usually points towards an inflammatory process (post traumatic or infective). Other ‘non inflammatory lumps’ exist, with the most likely differential diagnosis being benign soft tissue tumours. These lumps however are unlikely to cause pain. Our case presentation did not fit either of these clinical pictures, with symptoms lying between the two broad diagnostic categories [4, 5].
Imaging still remains the gold standard for diagnosis. Plain radiographs are usually the first modality and will display a well-defined intramedullary lesion with sclerotic margins (specificity 37%, Sensitivity 73%). MRI offers high sensitivity with a ‘four layer target appearance’ or ‘penumbra sign’ [6].
Staphylococcus aureus is the most common organism isolated, however it is only isolated in as few as 75% of cases. Treatment of a Brodie’s abscess has no agreed comprehensive guidelines, however long-term antibiotics is widely accepted [3, 7]. With regards to our case, the requirement for surgical drainage of a Brodie’s abscess while highly unusual was indicated. It aimed to be curative but also to provide symptom relief.
This case highlights a very unusual presentation of a Brodie’s abscess. We believe this to be the first reported case of an abscess forcing a cloaca into soft tissues, causing an extensive purulent collection. We also highlight how problematic management of complex loculated abscess’ can be. It is standard practice to drain abscesses and primarily close the skin layer, however, in this case it was felt prudent at the second procedure to modify the technique. The use of a ‘wick’ may have promoted resolution of the infection and should be something to consider in the future.
CONFLICT OF INTEREST STATEMENT
None declared.



