-
PDF
- Split View
-
Views
-
Cite
Cite
Nicolas Berte, Alya Filfilan, Laurence Mainard, Ludovic Mansuy, Jean-Louis Lemelle, Co-existing infantile hepatic hemangioma and mesenchymal hamartoma in a neonate, Journal of Surgical Case Reports, Volume 2018, Issue 1, January 2018, rjx260, https://doi.org/10.1093/jscr/rjx260
Close - Share Icon Share
Abstract
Infantile hepatic hemangioma (IHH) and mesenchymal hamartoma (MH) form the first and second most common benign hepatic tumors in children. In this case report, we present a newborn child in whom a growing hepatic mass was discovered at the age of 7 days. She suffered also from anemia, respiratory and renal failure. No signs of heart disease or cutaneous lesions were detected. Alpha-fetoprotein was elevated for her age (3562.2 ng/ml). Imaging studies showed multifocal large cystic lesions associated with heterogeneous small solid lesions with arterial enhancement of the liver. Non-anatomical liver resection was performed initially and synchronous MH and IHH GLUT-1 positive were discovered in the pathological analysis. Segmental IV hepatic resection and later on selective cysts excision were done for persistent hepatic lesion despite medical treatment. After 14 months of beta-blockers treatment, clinical follow-up shows a healthy child with no residual cystic lesions.
INTRODUCTION
Benign hepatic tumors form one-third of all hepatic lesions. Infantile hepatic hemangioma (IHH) was found to be the most frequent benign hepatic tumors followed by mesenchymal hamartoma (MH), focal nodular hyperplasia (FNH), nodular regenerative hyperplasia (NRH) and hepatic adenoma (HA) in a decreasing order [1]. Although deficiently reported in the literature, the rare co-existence of hepatic hemangioma and MH could be found in pediatric age group. This rare association might be considered as incidental or real concurrence between the two pathologies [2].
CASE REPORT
We present a currently 34-month-old girl, born prematurely at 35th week of gestation due to fetal distress. The mother was diagnosed with pre-eclampsia during her pregnancy which eventually mandated the preterm delivery. However, neither fetal abnormalities nor hepatic lesions were detected prenatally. At the age of 7 weeks (42nd week of corrected date), the child presented with massive abdominal distention reported by the family to be progressively growing since birth. Clinical examination revealed pale tachypneic afebrile child with severely distended abdomen with huge hepatomegaly causing severe respiratory distress and bowel obstruction. No infantile jaundice, dysmorphic features, cutaneous lesions nor other stigmata of liver disease were found. The child was admitted in the neonatal intensive care unit.
Abdominal ultrasound showed enlarged liver with multi nodular hypo-hyperechogenic hepatic lesions with complete distortion of hepatic vasculature. Computed tomography (CT) scan with contrast injection showed co-existing multifocal hepatic solid and macro-cystic lesions with no hepatic calcifications (Fig. 1).
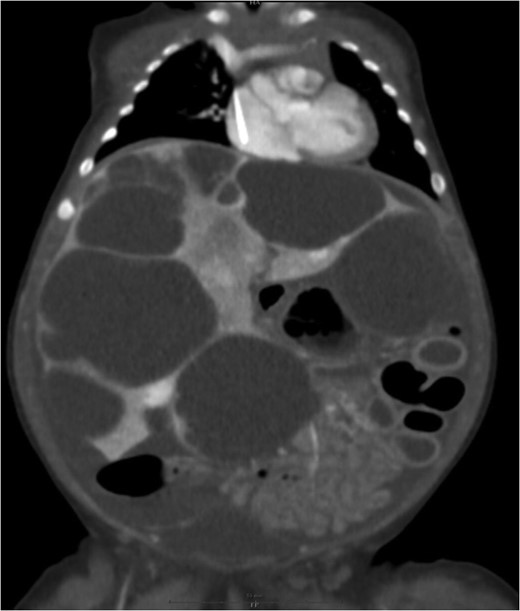
Large cystic lesions with internal septation associated with heterogeneous small solid lesions with arterial enhancement.
Measurement of human chorionic gonadotropin was within the normal range while alpha-fetoprotein was elevated for her age (3562.2 ng/ml). Random needle transcutaneous biopsies were done but unfortunately, histopathological examination was inconclusive.
Three days later, the patient developed a sudden abdominal compartment syndrome (hemodynamic instability, respiratory and renal failure). Urgent laparotomy and decompressing non-anatomical resection through a bilateral subcostal incision was performed. Four hepatic cysts were excised, two from the right and two from the left liver lobe while many other small non-compressive cysts were not excised. The removed cysts measured between 4 and 9 cm in diameter and between 46 and 300 g in weight (Fig. 2).
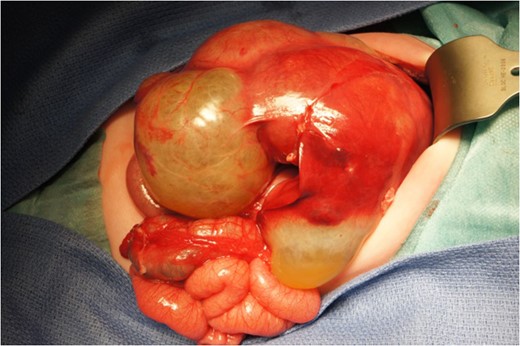
Surprisingly, microscopic analysis of two excised cysts among four showed complex lesions of HR containing multi centric zones of infantile hemangioma staining positively for glucose transporter-1 (GLUT-1+).
Medical treatment was started immediately with intravenous corticoids (2 mg/kg/day) accompanied with beta-blockers (propranolol 2 mg/kg/day). Ultrasound and CT scans performed after 6 months showed scattered liver parenchymal invaded by multiple enlarging cysts varied in sizes and shapes and causing severe abdominal compression (Fig. 3).
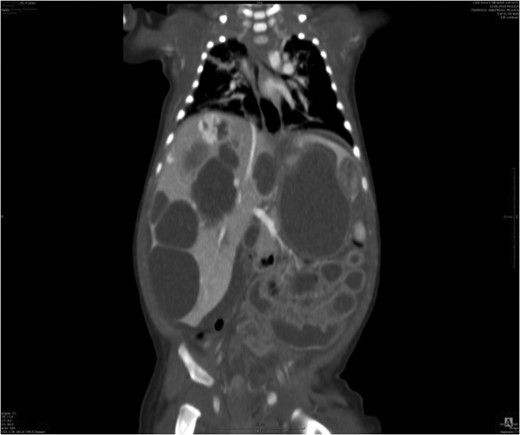
Liver parenchyma invaded by multiple enlarging cysts varied in sizes and shapes.
Segmental IV hepatectomy was performed after 8 months of the first operation. Histopathologic analysis of the tumor showed again the same complex lesion of HR containing infantile hemangioma GLUT-1+ without any signs of malignancy.
The remaining lesions of IHH were treated by large dose of beta-blockers and regressed significantly. However, another subcapsular cystic lesion developed after 6 months from the second operation. Selective surgical excision was performed this time for the newly developed cystic lesion and medical treatment was continued. Today, at the age of 34 months, the child carries a good general condition with satisfying tolerance to her beta-blocker treatment. Ultrasonographic follow-up shows normal regenerative liver parenchyma with a small hemangiomatic lesions measuring <1 cm.
DISCUSSION
Benign liver tumors count for one-third of all hepatic lesions [3] while malignant lesions, primarily metastasis, form the other two-thirds. Many studies showed that among these benign lesions, IHH represent the most common benign tumor of the liver in children mostly in the first 6 months of life and accounts for 12% of all pediatric lesions. MH of the liver form 8% of benign lesions and presents frequently as an enlarging mass in the young children. Nearly 85% of hamartoma lesions occur in children under 2 years of age and rarely above the age of 5 [1]. However, the association between these two lesions is exceptional and extremely rare in pediatric age group [2]. The lesion in these three patients presented differently than our case. The first child had synchronous lesions of IHH and MH but was separately located in the liver while in the second case; IHH appeared 6 months after of the surgical treatment of MH. In the third case, they were located in the same extensive tumor, but IHH was GLUT-1 stain was negative.
Bejarano et al. [4] reported a case of a newborn girl who underwent surgical resection or large lesion of MH while IHH developed lately after 4 months of the excision.
Kuang-Hung et al. [5] also conducted a case of a female newborn that had a hepatic mass detected prenatally. Segmental resection was performed initially and complete resection of these tumors and left lobectomy were performed 21 days later. Pathological examination showed synchronous lesions of MH and IHH of the same lobe.
This case report shows a lot of similarity to our case but managed differently. We performed repeated non-anatomical resections in association with medical treatment for IHH (steroids and beta-blockers in large doses) while Kuang-Hung et al. performed only anatomical lobectomy without medical treatment reported. Furthermore, no information was given about histochemical staining for GLUT-1 in their study.
Our management composed of both surgical and medical treatment. First surgery permitted us to obtain decompression and histopathological diagnosis. Discovery of IHH lesions in histopathological analysis indicated medical treatment with beta-blockers. The second and third tumor resections were mainly performed for the recurrence of lesions and non-responsive to medical treatment. This management helped in minimizing the advanced liver resection and regeneration of hepatic parenchyma.
Synchronous IHH and MH are exceptional situations. Its treatment could include both medical (beta-blockers) and surgical excision. Non-anatomical tumor resection in large lesions, even in clinically unstable patients and programmed secondary resection for persistent non-responsive lesions in optimal clinical situation could be a considerable option permitting good preservation and regeneration of liver parenchyma in case of benign extended tumors.
CONFLICT OF INTEREST STATEMENT
None declared.
REFERENCES
- anemia
- beta-blockers
- heart diseases
- alpha-fetoproteins
- benign hepatic neoplasms
- kidney failure
- hemangioma of liver
- heterogeneity
- child
- cysts
- follow-up
- hepatic resection
- newborn
- diagnostic imaging
- liver
- skin lesion
- persistence
- well child
- mesenchymal hamartoma
- glut-1
- excision
- liver mass
- hepatic lesions
- medical management



