-
PDF
- Split View
-
Views
-
Cite
Cite
Santiago A Endara, Fernando J Terán, Armando J Serrano, Manuela J Castillo, Gabriel A Molina, Esophagocoloplasty fistula successfully treated with vacuum-assisted closure, Journal of Surgical Case Reports, Volume 2018, Issue 1, January 2018, rjx256, https://doi.org/10.1093/jscr/rjx256
Close - Share Icon Share
Abstract
Esophageal fistulas in the cervical region are usually difficult to manage and carry a high morbidity. We report a case of an esophago-colonic fistula after colonic interposition, successfully managed with vacuum-assisted closure ‘V.A.C. system’, (Kinetic Concepts Inc., San Antonio, TX, USA). The patient initially presented with purulent fluid from the cervical wound 13 days after surgery. Esophagogram confirmed a leak. Since the patient had a history of anastomotic leaks, a surgical intervention was not the treatment of choice. In light of this, conservative treatment with V.A.C. system was initiated. She underwent full recovery.
INTRODUCTION
Colon interposition is a reliable esophageal replacement; colon provides an extended conduit length, reliable blood supply and low incidence of reflux [1]. Anastomotic leak presents in 10–25% in the cervical region but mortality rate in this region is low 4% [2]. Leakage of cervical anastomosis defeats the primary objective of esophageal reconstruction since the patient cannot eat. The etiology of anastomotic leaks is multifactorial including systemic diseases, esophagus anatomy and operative factors [3]. Management of cervical leaks may be treated with drainage, daily bedside dressing, antibiotics, total parental nutrition [4] and surgical procedures.
We present a case of an esophagocoloplasty anastomotic leak successfully treated with V.A.C. system.
CASE REPORT
Patient is a 51-year-old woman with past medical history of hypothyroidism. She was complaining of dyspepsia so an upper endoscopy was done, revealing a mass in the greater curvature of the stomach, and a biopsy was taken. Pathology showed a poorly differentiated infiltrating adenocarcinoma with signet ring cells. A total radical gastrectomy reconstructed with esophagojejunal Roux-en-Y anastomosis was done. On the sixth postoperative day, purulent drainage was seen on the abdominal drain. And, an abscess was discovered at the level of the esophagojejunal anastomosis, surgery was required, the abscess was drained and a new esophagojejunal anastomosis was done high in the chest with autosutures. The patient persisted with poor medical condition; so an esophagogram identified a leak at the level of esophageal anastomosis, and after failed endoscopic placement of two metal stents to solve the leak, patient persisted with sepsis. Redo operation was performed and at thoracotomy an anastomotic leak, with free purulent fluid in the pleural cavity was found (Fig. 1A). An exhaustive washing of the pleural cavity was performed, stents were removed, thoracic esophagectomy was done, a feeding jejunostomy was made and a cervical esophagostomy was performed. Patient improved considerably after this, with adequate nutritional management through jejunostomy. She was discharged, and 6 months later she was hospitalized again for intestinal transit restitution with an esophagocoloplasty with interposition of the right colon via substernal route.
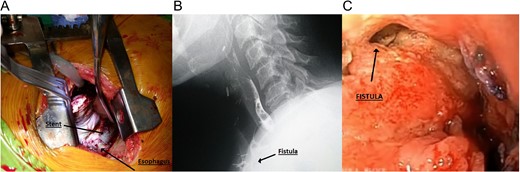
(A) Metal stent seen during thoracotomy. (B) Cervical fistula seen during esophagogram. (C) Cervical fistula seen during upper endoscopy.
Esophagocoloplasty was done, and hand-sewn anastomoses were made between the esophagus and the colon, drains were left in the abdomen and neck.
On the 10th postoperative day, an esophagogram was done to assess the neck anastomosis, which did not show any leakage or stenosis, which is why sips of liquids were initiated, attaining good oral tolerance, antibiotics were withdrawn, abdominal and cervical drains were removed and soft diet was initiated.
On the 13th postoperative day, serous fluid drained through the neck and became purulent a day after. A new esophagogram was done and an esophago-colonic anastomosis leak was discovered (Fig. 1B). An upper endoscopy was performed, localizing the fistula of 12 × 6 mm (Supplementary Video & Fig. 1C).
Plastic surgery consultation was requested; management of the fistula with V.A.C. was decided.
Partial opening of the cervical wound was done, and necrotic tissue debridement with extensive irrigation of the wound with saline and iodine over the cervical esophagus was performed. After this to protect the esophago-colonic anastomosis from direct contact with the V.A.C. a small paraffin gauze dressing (Lomatuell H, Paraffin Gauze Dressing) was placed over the cervical esophagus. The V.A.C. sponge was fashioned to fit the wound and placed over it. The adhesive drape was fixed to the neck skin and continuous suction between 100 and 125 mmHg was installed (Fig. 2A). In the first week, V.A.C. system drained about 50cc of saliva-like fluid daily and was changed every 2 days, once granulation tissue had begun to form over the wound, the system was changed every 5 days and no paraffin gauze was used (Fig. 2B). All V.A.C. changes were done in the operating room and during the first week of V.A.C. treatment, patient received total parental nutrition, on the 10th day patient was able to ingest liquids. Twelve days after initial use, the leak closed, since no fluid came out of the V.A.C. system, and after the patient resumed full normal diet, she was discharged home. On follow-up controls, the patient was in good condition (Fig. 2C).

(A) Functional V.A.C. system in-patient. (B) Granulation tissue in the cervical wound. (C) Wound after therapy.
DISCUSSION
The etiology of esophageal anastomotic leaks is multifactorial [1]. Our patient had hypothyroidism and gastric cancer that may have contributed to the development of anastomotic leaks. The initial presence of fistula was based on the clinical findings and verified with an esophagogram.
The use of negative pressure wound therapy healing consists of a hydrophobic sponge, connected to a device that produces a negative pressure over the wound [6]. V.A.C. therapy is a unique wound management system specifically designed for wounds through the application of negative pressure [7]. Since, it was first described by Argenta in 1997 and introduced in USA, (V.A.C., KCI, San Antonio, TX) as a commercial product the number of indications for the V.A.C. system has steadily increased [5].
Applications of V.A.C. on a wound provide better infection control, faster wound healing, improved comfort of patients, decreased workload for the medical team and less need for an advanced reconstruction. V.A.C. therapy is a useful modality to manage wounds in the head and neck [8]. For these reasons, we attempted to treat an esophago-colonic fistula in a patient with a past medical history of leaks.
The major advantages of the V.A.C. system are the no need of a nasogastric tube for decompression, no need of a nasoenteric tube for feeding, the possibility to maintain oral diet and no need of frequent daily dressing changes [9]. In our patient, therapy lasted 12 days; in other publications, the duration of this treatment was similar, with a minimum of 6 days to a maximum of 18 days [1].
There are reports of V.A.C. in cervical leaks after gastric pull up [9], however, after an extensive search we have not found the use of V.A.C. in this kind of fistula.
Complications following colon interposition may be difficult to treat. Creative strategies are needed to salvage or help in wound healing when the anastomosis is compromised, we strongly suggest applying V.A.C. therapy in esophago-colonic fistulae.
SUPPLEMENTARY MATERIAL
Supplementary material is available at the Journal of Surgical Case Reports online.
CONFLICT OF INTEREST STATEMENT
None declared.



