-
PDF
- Split View
-
Views
-
Cite
Cite
Osama Elhardello, Basil J Ammori, Splenic pedicle control during laparoscopic de-capsulation of a giant splenic cyst, Journal of Surgical Case Reports, Volume 2018, Issue 1, January 2018, rjx255, https://doi.org/10.1093/jscr/rjx255
Close - Share Icon Share
Abstract
Splenic cysts are a rare entity in the Western population and are either true cysts (primary, 25%) or pseudocysts (secondary, 75%) complicating trauma, haemorrhage or infarction. Congenital or simple splenic cysts are the commonest primary cysts and surgery is recommended for cysts larger than 5 cm as these are prone to infection, bleeding or rupture and for symptomatic or complicated cysts. Splenic preservation techniques using the laparoscopic approach are the most prevalent. We present a case of a giant painful simple splenic cyst treated with laparoscopic de-capsulation with application of a new technique for achieving vascular control, whereby control of the splenic pedicle was achieved using a Nylon tape. This approach was safe and well tolerated with a total splenic ischaemia time of 30 min and a successful result. The patient was discharged with no antecedent complications and no recurrence of the cyst at 6 months follow up ultrasound scan.
INTRODUCTION
Splenic cysts are rare, particularly in the West [1], with around 1000 cases reported in the literature. Pathologically they are classified as true cysts (primary, 25%) that are lined by epithelium or false cysts (secondary or pseudocysts, 75%) without endothelial lining and are often secondary to trauma, haemorrhage or infarction. True cysts can be further subdivided based on aetiology into parasitic, neoplastic or congenital [2, 3].
Congenital cysts are benign, sporadic, have a slight female preponderance and with an unclear pathogenesis [4]. Most of these are asymptomatic and present at an early age as an incidental radiological finding in the upper pole of the spleen. Clinical presentation is observed with cysts larger than 5 cm as these are prone to infection, haemorrhage or rupture. Surgery is recommended for cysts larger than 5 cm, symptomatic or complicated cysts [2].
Computed tomography (CT) scan, ultrasound scan and magnetic resonance imaging (MRI) are useful imaging modalities to describe the cyst and its relation to the spleen and surrounding structures [5]. The definitive diagnosis lies with histopathologic analysis of the resected cyst [5].
Management is mostly surgical and include aspiration, marsupialization, cystectomy, cyst de-roofing, cyst de-capsulation, partial splenectomy and splenectomy. Laparoscopic de-capsulation involves a near total cystectomy with removal of the visible cyst wall and it’s contiguous splenic parenchyma, leaving the very adherent part that cannot be denuded off the spleen [1, 4]. Current surgical trends are towards splenic preservation surgery to avoid post-splenectomy complications and laparoscopic techniques [6, 7]. Factors dictating the use of one procedure or another are the number of cysts as well as size and location in relation to the splenic hilum and the major splenic vessles [8]. Care should be taken when considering the differential diagnosis to rule out echinococcal cysts, using a combination of cross-sectional imaging and serological testing as these should be dealt with carefully and preferably by open surgery to avoid spillage into the peritoneal cavity and dissemination.
CASE REPORT
A 19-year-old female presented with a 2-day history of severe left upper abdominal pain. There was no known history of abdominal trauma or travel outside the UK. She was systemically well, had a soft abdomen with exquisite tenderness at the left upper quadrant and loin regions. The provisional blood tests, hydatid serology and chest and abdominal X-rays were unremarkable. An ultrasound scan showed a large splenic cyst with no increase in vascularity on Doppler assessment, while an intravenous contrast-enhanced CT scan showed a 12.5 × 9.7 × 10.7 cm well-defined cystic mass arising from the upper pole of the spleen (Fig. 1) with multiple fine echogenic shadows and medial displacement of the stomach and the left kidney (Fig. 2). Findings were consistent with the diagnosis of a simple splenic cyst. The patient was scheduled for an urgent laparoscopic de-capsulation, and received triple vaccination (meningococcal, pneumococcal and Haemophilus influenzae type B). Although 2 weeks are recommended between vaccination and splenectomy should this be needed, we proceeded to surgery after 10 days from vaccination as the patient was considerably troubled with abdominal pain and we were confident that a total splenectomy could be avoided.
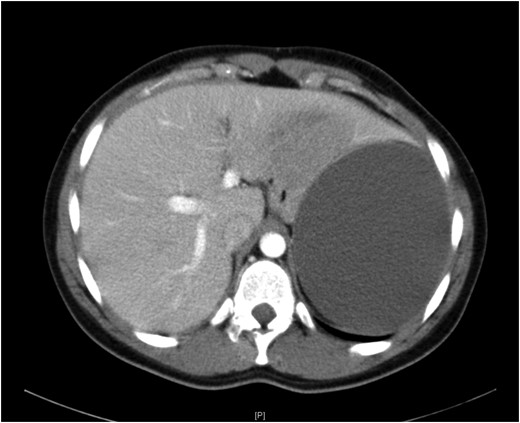
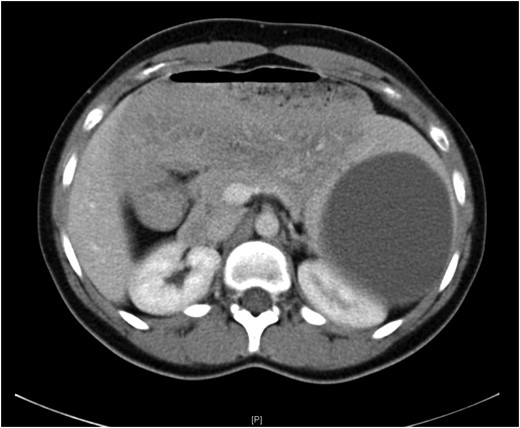
Computed tomography showing medial displacement of the stomach and the left kidney by the cyst.
Under general anaesthesia, the patient was placed in the right lateral position. Laparoscopic surgery proceeded with four ports in the left upper abdomen (Fig. 3). Then under 15 mmHg capnoperitoneum, the spleen was retracted using a 5-mm diamondflex retractor (Lina Medical, Devon, UK). A large simple–appearing splenic cyst was demonstrated, arising from upper pole of the spleen, with some inflammatory adhesions to the under surface of the left lobe of liver and diaphragm. The splenic hilum was exposed after dividing the gastrospelnic ligament and the hilar vessels were slung in a Nylon tape. The adhesions were divided using the Thunderbeat coagulation device (Ethicon, Livingston, UK). The slung splenic hilum was clamped by advancing a plastic tube (a mid-section of a nasogastric tube) over the Nylon sling and fixing it in position with a haemostat applied outside the abdomen (Fig. 4). The cyst was then decompressed by aspirating its clear straw-coloured fluid content which enhanced exposure and access. De-capsulation of the cyst was performed using the Thunderbeat coagulation device to include the thinned part of the spleen over the cyst, with removal of ~90% of the cyst wall. The remainder of the intra-splenic portion of the cyst wall was sprayed with diathermy to destroy its lining epithelium. The splenic edge was treated with Floseal Haemostatic Matrix (Baxter Helathcare S.A, Zurich, Switzerland) and a sheet of Surgicel (Gelita Medical, Eberbach, Germany) was applied to an oozy part and was oversewn over the spleen edge with Vicryl 4/0 in a continuous manner. The hilum was unclamped after a total ischaemia time of 30 min and no bleeding was encountered despite reducing the intraperitoneal pressure to 7 mmHg for 3 min. The spleen appeared well perfused (Fig. 5).
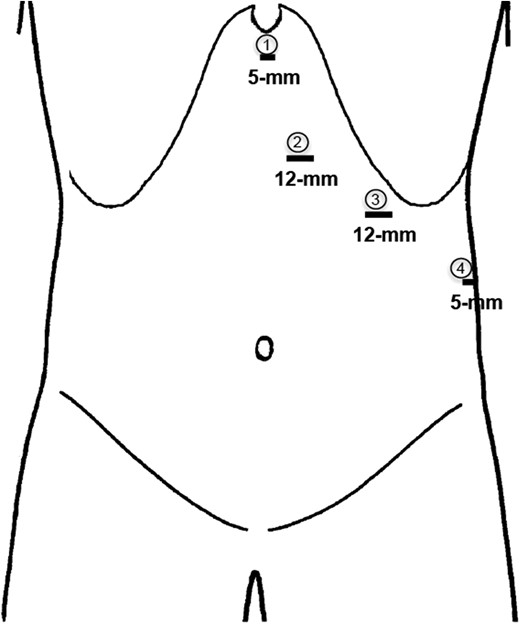
A schematic illustration of the ports positions. The working ports are numbered 1 and 3, port 2 is for the laparoscope, while port 4 is for a 5-mm diamondflex retractor.
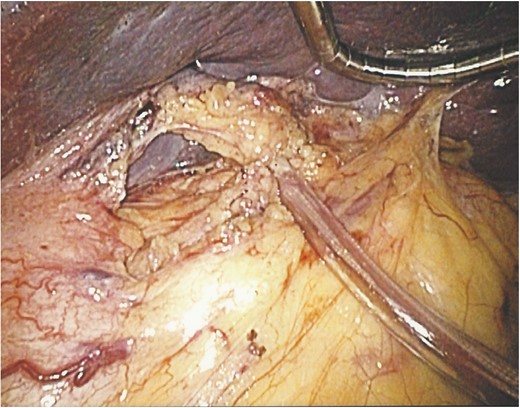
An operative image showing the splenic hilum slung with the vascular tape and clamped with a segment of a nasogastric tube.
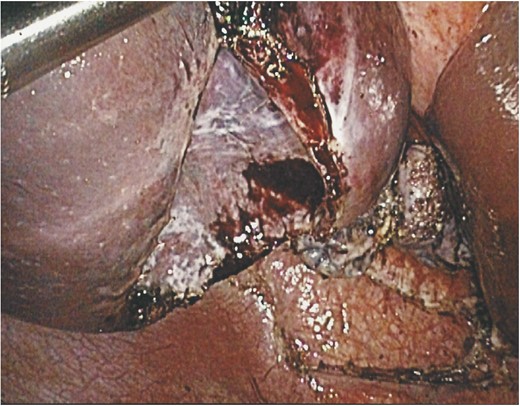
An operative image showing the splenic cyst after de-capsulation with a bloodless bed and minimal bleeding from edges of the cyst.
The patient made an uneventful recovery and was discharged on the third post-operative day. The histopathology confirmed a primary cyst with no evidence of malignancy. She remains asymptomatic 6 months after surgery when an ultrasound scan showed a normal spleen with no evidence of recurrence.
DISCUSSION
The conventional treatment of simple splenic cysts has been splenectomy, either open or laparoscopic. This would achieve a complete extirpation of the cyst with avoidance of recurrence. Different laparoscopic spleen preserving procedures were described recently such as partial splenectomy, cyst marsupialization, cyst de-roofing and cyst de-capsulation [8]. Laparoscopic de-capsulation which was done here is simpler and quicker to perform with less blood loss than partial splenectomy, there is a small possibility of recurrence as a portion of the cyst lining is left in situ. The recurrence rate as reported in small series was lower than aspiration and marsupialization and is dependent on the amount of cyst lining left behind [3].
In this report, we describe for the first time a new approach that involved slinging and clamping the splenic hilum on a vascular tape, which enabled a bloodless approach to a radical de-capsulation without the need to tackle smaller arterial branches, avoided tedious bleeding that could have obscured the surgical field, and avoided taking down small arterial branches with the potential of segmental infarction of the spleen. This manoeuvre resembles in principle the Pringle manoeuvre [9] commonly used in liver resection. This approach can be added to the armamentarium of the laparoscopic surgeon to simplify a more radical resection of simple splenic cysts.
CONFLICT OF INTEREST STATEMENT
None declared.



