-
PDF
- Split View
-
Views
-
Cite
Cite
Joshua Henry, Alistar J Konarski, Leena Joseph, Anand Pillai, Foreign body reaction with granuloma following Achilles tendon reconstruction with the LARS ligament, Journal of Surgical Case Reports, Volume 2018, Issue 1, January 2018, rjx258, https://doi.org/10.1093/jscr/rjx258
Close - Share Icon Share
Abstract
Ligament reconstruction with the LARS ligament has been a popular choice owing to its low-complication rates compared with previously commercially available grafts. The non-active nature of the implant also meant that there were no foreign body reactions that had been described with other synthetic grafts. We describe the first reported case of a granulomatous foreign body reaction in a LARS ligament Achilles tendon graft and a technique to reconstruct the tendon following its excision.
INTRODUCTION
Synthetic grafts for soft tissue reconstruction became popular in the 1980s but fell out of favour due to complication rates. The Ligament Advanced Reconstruction System (LARS) ligament has been shown to be effective in a variety of uses, most commonly in anterior cruciate ligament reconstructions, but also in Achilles tendon repairs. Several studies have demonstrated low-complication rates with no foreign body reactions that had previously been seen with other synthetic grafts [1]. We report a rare case of a granulomatous reaction to a LARS Achilles Tendon graft and describe a successful method of reconstruction following its excision.
CASE REPORT
A 68-year-old man was referred to us with swelling around the right Achilles tendon. He had ruptured his Achilles 14 years previously which was repaired using a LARS ligament. The swelling had increased over a period of the past 12 months with associated pain and difficulty wearing footwear. On examination, there was a large cystic swelling, but no inflammatory skin changes or discharge to suggest an infection (Fig. 1).

An MRI scan showed a 10 × 3.6 × 3 cm collection within the Achilles tendon that was thought to be an evolving haematoma, along with debris in the periphery. Continuity of the Achilles was demonstrated (Fig. 2).

MRI scan. T2 PD fat sat sequence sagittal image of right ankle showing high-signal collection within the Achilles tendon.
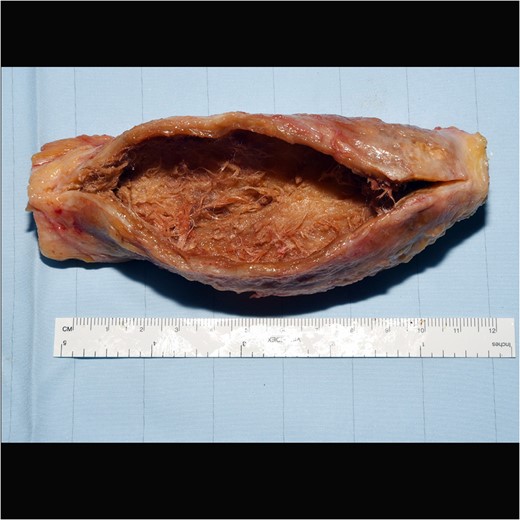
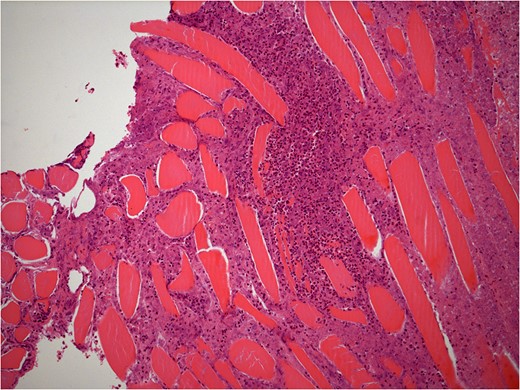
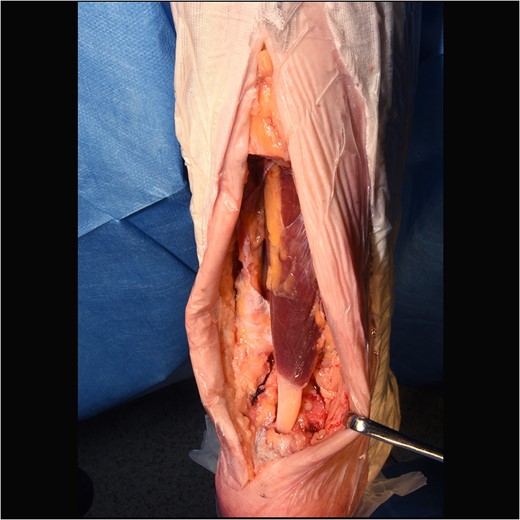
He underwent surgery to explore the tendon where an irregular, cystic, fibrofatty lesion was identified within the tendon (Figs 3–5). This was successfully resected and sent for histology which showed a florid granulomatous and histiocytic response to the suture material, in keeping with a suture granuloma (Figs 6 and 7). There was histological evidence of the abscess extending into the muscle (Fig. 8).
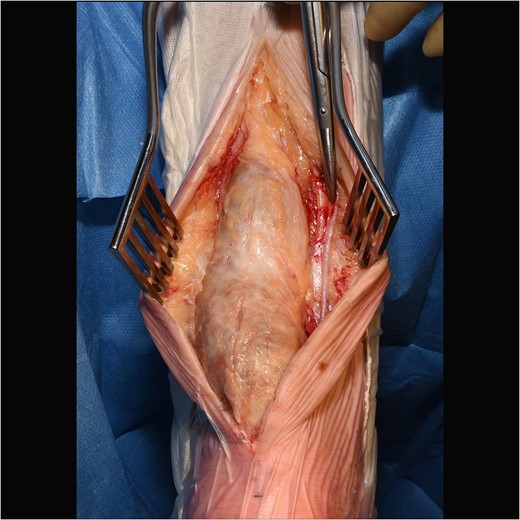
Intraoperative image of large cystic swelling over Achilles tendon.
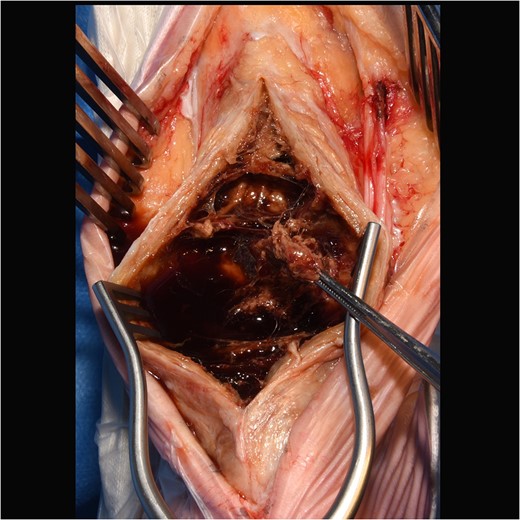
Intraoperative image showing internal cystic granuloma within Achilles.
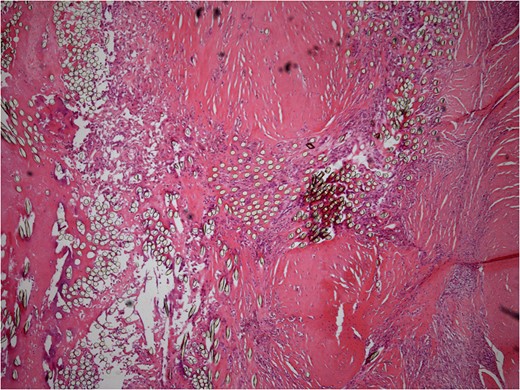
Low power histology slide showing foreign body giant cell reaction to suture material.
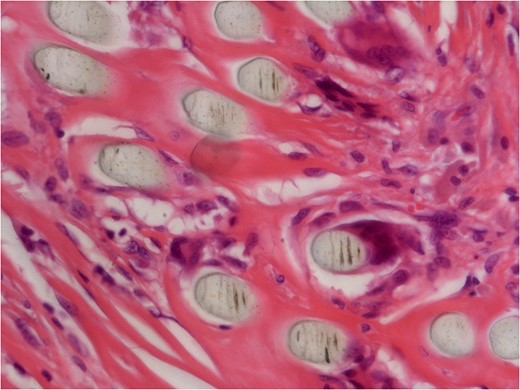
40× histology slide showing foreign body giant cell reaction to suture material.
We then reconstructed his Achilles tendon using an Flexor Halluces Longus (FHL) transfer (Fig. 9). The patient recovered well from his surgery with no current complications.
DISCUSSION
Synthetic ligaments became popular in 1980s and 90s for a variety of soft tissue reconstruction and repair techniques; however, multiple problems including high failure and revision rates, foreign body reactions, synovitis and early onset osteoarthritis caused a restriction in their use [2]. Further developments led to second and third generations of synthetic graft materials, including evolution from non-biological to biological grafts. One of these developments is the LARS ligament. These ligament reconstructions have been used now for over 20 years. The structural component consists of polyethylene tetraphthalate and various designs have been made to closely recreate ligamentous anatomy. They are non-active surgical implants, but allow fibroblast ingrowth and have been licensed for use in a variety of applications, including anterior and posterior cruciate ligament reconstruction, ankle and shoulder repairs.
The majority of the available literature is focused on its use in ACL surgery, with many studies demonstrating good surgical outcomes and patient satisfaction [3, 4]. Histological studies have shown cellular and connective tissue ingrowth into the LARS ligament [2]. A systematic review by Chen, of commercially available scaffold products for ligament and tendon reconstructions analysed six studies looking at the use of LARS ligaments, all in the knee. They concluded that the LARS was the most efficient synthetic scaffold for tendon repair with the available studies supporting its use. It commented that while studies into other synthetic scaffolds such as Leeds-Keio, and Gore-Tex, had reported major complications including synovitis, osteolysis and foreign body reaction, these had not been found in any of the studies into LARS [5].
LARS ligaments are also licensed for use in Achilles tendon repair, although there is less literature on this use. One study found that it gave good outcomes when used for the management of chronic Achilles tendon ruptures [6]. The retrospective case series of 14 patients, with 3-year follow-up, showed good outcomes measured on the American Orthopaedic Foot and Ankle Society (AOFAS) ankle and hindfoot scoring system, and the Tegner Activity Scale. They reported no foreign body reactions, with only one superficial wound infection. Another case report by Dhillon demonstrated its use in a bilateral Achilles tendon rupture that reported a good functional outcome, but was complicated by significant wound healing problems [7].
Our case is the first reported case of granulomatous change in a LARS ligament used for an Achilles tendon repair. A small case series of revisions for failed LARS ACL reconstructions found one patient who had demonstrated a foreign body synovitic reaction, similar to the one described in our case and to our knowledge is the only other report of this type of reaction to a LARS ligament [8]. A study by Ventura analysed the synthetic ligaments in patients undergoing revision of a synthetic ACL reconstruction. Although the study did not include any LARS ligaments, it included three others (Treviratochfest, Proflex and Pro-Pivot) that were also made of polyethylene tetraphthalate. On histological analysis of the removed grafts, it found that they showed signs of foreign body granulomatous reactions and giant foreign body cells [9]. It is thought that the foreign body reactions in other studies started from wear particles which lead to an inflammatory reaction [5].
Synthetic grafts offer the advantage that they are manufactured, allowing better control over their physical properties and consistency. The disadvantage is that they are synthetic and therefore are not truly biocompatible, and so have an associated risk of an inflammatory response from the host.
While this is the first reported case of granulomatous change in a LARS ligament used for Achilles reconstruction, other studies have shown that this can occur in other synthetic ligament reconstructions. This should be considered for patients with symptoms following reconstruction surgery with a LARS ligament and taken into consideration when planning Achilles tendon repairs. We have also demonstrated that en bloc resection and reconstruction with FHL transfer is an effective treatment method.
CONFLICT OF INTEREST STATEMENT
None declared.



