-
PDF
- Split View
-
Views
-
Cite
Cite
Tian Ran Zhu, Jonathan Bass, Scott Schmidt, Surgical management of digital ischemia caused by constriction band formation in a patient with ichthyosis vulgaris, Journal of Surgical Case Reports, Volume 2017, Issue 9, September 2017, rjx183, https://doi.org/10.1093/jscr/rjx183
Close - Share Icon Share
Abstract
Ichthyosis is a broad and loosely defined group of hereditary and acquired disorders characterized by filaggrin dysfunction and impaired epidermal homeostasis that results in dry, scaly and thickened skin. Individuals with truncation mutations in the profilaggrin gene coding for filaggrin are strongly predisposed to severe forms of ichthyosis. The phenotypical expression of ichthyosis caused by the same genotypical mutation can vary considerably in severity and in regards to how much constricting scar tissue develops. Here, we report a case of digital ichthyosis threatening the neurovascular integrity to the small finger to discuss the importance of early diagnosis and role of Z-plasty flaps in the surgical treatment of constriction band formation.
INTRODUCTION
Ichthyosis is a heterogenous family of cutaneous disorders characterized by dry, scaly, skin, erythema, blistering or excessive skin desquamation. The term ichthyosis comes from the Greek root ichthys, meaning fish, which describes the pathologic state of abnormal keratinization resembling fish scales [1]. Ichthyosis may be either inherited or acquired. Inherited ichthyosis is often caused by autosomal dominant mutations resulting in loss of filaggrin, which leads to compensatory inflammation, epidermal hyperplasia and aberrant desquamation resulting in excess water loss and hyperkeratosis [2, 3]. Consequently, the impaired barrier predisposes the individual to increased sensitization of exogenous allergens with increased propensity for inflammatory skin diseases and secondary bacterial infections [4].
The most common type of ichthyosis is ichthyosis vulgaris, which accounts for more than 95% of ichthyosis cases. It frequently manifests in early childhood, often at birth, and continues to affect a person throughout life. Most clinical presentations of Ichthyosis vulgaris have been described to involve upper and lower extremities encompassing a wide clinical spectrum from mild flaky scaling patches to hyperlinearity of palms and soles to more severe hyperkeratotic plaques with fissures on palmoplantar skin [1, 5, 6]. The diagnosis of ichthyosis vulgaris is established clinically and therapy is multifactorial incorporating hydration, lubrication and keratolytic agents, as well as topical antibiotic prophylaxis against secondary infection [7]. Because normal cycles of skin turnover are disrupted in ichthyosis vulgaris, agents that restore and maintain hydration of the epidermis are critical in facilitating scale removal and epithelial homeostasis [7–9]. However, when severe hyperkeratosis results in circumferential contracture bands that threaten neurovascular integrity of digits and/or limbs, surgical intervention is necessary to prevent irrevocable tissue necrosis and subsequent auto-amputation.
CASE
A 14-year-old female with ichthyosis vulgaris presented with a recurrent right small finger proximal interphalangeal (PIP) joint constriction band with significant swelling distal to the constriction site (Figs 1 and 2). The patient has a family history notable for a father with multiple digits amputated secondary to a similar process. The patient had previous surgeries for digit contracture release over the course of 7 years beginning with her first operation at age 6. The patient is otherwise healthy and reports no concurrent medical conditions. Examination of her upper extremities by manual palpation and use of hand-held Doppler ultrasound revealed an intact pulse along ulnar and radial distribution of right small finger. Light touch, two-point tactile stimulation and sharp–dull discrimination exhibit mild decline in median and ulnar dermatomal distribution.
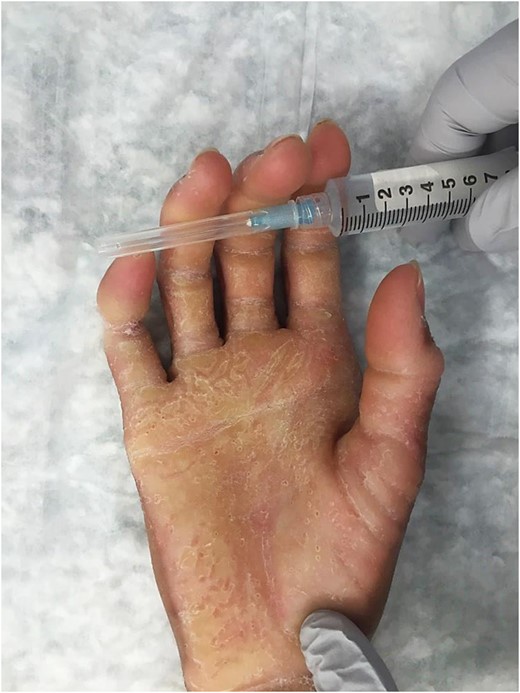
Preoperative. Right hand (volar) showing palmar and digital hyperkeratotic scales and circumferential constriction band on right small finger around proximal interphalangeal joint.

Preoperative. Right hand (dorsal) showing hyperkeratotic scales on metacarpal phalangeal and proximal interphalangeal joints of first three digits and circumferential constriction band on right small finger around proximal interphalangeal joint.
The patient was brought to the operating room, prepped and draped in the usual sterile fashion, and anesthesia was initiated. The patient’s right small finger constriction band was excised in a full-thickness fashion, with careful attention paid not to injure the underlying dorsal vein or extensor and flexor tendons volarly (Fig. 3). A series of multiple Z-plasties with six transposition flaps were elevated and transposed and sutured in a circumferential fashion (Fig. 4). The tourniquet was let down and the capillary refill was noted distal to the operative site, demonstrating no evidence of venous congestion or tissue ischemia. Her right small finger was subsequently splinted with a plaster splint and covered in gauze dressing to immobilize both PIP and distal interphalangeal (DIP) joints in order to promote wound healing and minimize scar formation.

Surgical scalpel blade No. 15 was used to incise and elevate the constriction band circumferentially, taking care not to dissect too deeply to avoid injury to digital nerve and vessels.

Six Z-plasty transposition flaps incorporated for primary closure after constriction band release.
Patient was seen in clinic ~2 weeks after surgery and her splint and dressings taken down. Her right small finger surgical incisions were clean, dry and well-approximated along the Z-plasty closure lines without evidence of erythema, induration or drainage (Fig. 5). The patient demonstrated improved swelling distal to site of constriction band and diminished throbbing and discomfort. During this visit, she received physical therapy to help with managing pain, minimizing joint contractures, maximizing PIP and DIP flexion and extension motions, and increasing overall function of her right hand. Subsequent monthly follow-ups demonstrated continued improvement in her right small finger mobility and appropriate healing of her Z-plasty incisions.

Two weeks postoperative. Z-plasty incisions are well-approximated with scabs of crusted blood. Recurrence of hyperkeratotic scales disseminated on right volar hand.
DISCUSSION
The principal goal in the management of ichthyosis involves minimizing exacerbating factors, applying hydration promoting agents and administering antibiotics prophylaxis. Filaggrin is a critical protein integral to normal skin hydration as it incorporates within the lipid bilayer of the stratum corneum to form an impermeable barrier to water. However, when mutated, filaggrin results in impaired ability of the stratum corneum to retain water within skin, resulting in dehydration, hyperkeratosis and excess scar formation. Non-surgical therapeutic strategies including urea, salicyclic acids and alpha hydroxyl acids can be used to promote scale desquamation [10]. However, these medical modalities are limited in their efficacy to treat hyperkeratosis that results in significant constriction band around fingers and toes with subsequent auto-amputation.
Because it is difficult to diagnose early tissue ischemic changes before they become irreversible, we recommend a low threshold for initial surgical consultation and intervention at any sign of pain, skin discoloration or increased band firmness. Circumferential release and subsequent Z-plasty reconstruction have been described as a beneficial surgical approach in congenital constriction band [11, 12]. Other studies have reported that prompt surgical intervention resulted in limb salvage in patients with ichthyosis [13, 14]. This case describes the utility of multiple Z-plasty transposition flaps to effectively lengthen and reorient the scar lines to achieve tension-free closure, thereby decreasing the risk for future constrictive band. Additional research in filaggrin gene mutation and medical and surgical treatment modalities are needed to advance dermatologic care for patients with ichthyosis.
CONFLICT OF INTEREST STATEMENT
None declared.



