-
PDF
- Split View
-
Views
-
Cite
Cite
Khalid Alrabeeah, Ahmed Aljuhayman, Saad Abumelha, Mohammad Alkhamees, Noura Aloudah, Intra-scrotal testicular torsion of a classical seminoma in an elderly patient: a case report and literature review, Journal of Surgical Case Reports, Volume 2017, Issue 7, July 2017, rjx145, https://doi.org/10.1093/jscr/rjx145
Close - Share Icon Share
Abstract
Intra-scrotal testicular torsion of a seminoma is extremely rare and has been reported scarcely in literature. On the other hand testicular torsion by itself is rare in old age as well. We report a 63-year-old male who was presented to our Emergency Department with a right scrotal swelling and pain for 1 week. The patient had intra-scrotal testicular torsion of a seminoma which was overlooked initially by Doppler ultrasound, progression of symptoms led to a computed tmomgraphy scan which showed a testicular torsion. Intra-operative findings showed a torsed right testis with completely engorged cord. Right radical orchiectomy was done and indecently histopathology revealed a classical seminoma. Urologist should be aware and more vigilant of testicular torsion as a presentation of malignancy in old age especially with the presence of diagnostic limitations.
INTRODUCTION
Testicular torsion is defined as ‘ a rotation of the testis around the longitudinal axis of the spermatic cord, resulting in obstruction of testicular blood flow’, which accounts for 13–54% of acute scrotal disease [1]. Intra-scrotal testicular torsion as a presentation of malignancy is extremely rare especially in old age [2]. Whereas, intra-abdominal testicular torsion of malignancy has been described in the literature more widely [3–5]. We report a case of an intra-scrotal testicular torsion of a seminoma which was overlooked initially by Doppler ultrasound, progression of symptoms led to a computed tomography (CT) scan which showed a testicular torsion, the patient underwent radical orchiectomy and histopathology showed a classical seminoma. To our knowledge this is the first case of an intra-scrotal testicular torsion of a classical seminoma in a patient who is more than 60 years of age to be reported, not mentioning the unusual presentation of testicular torsion in a patient more than 60 years old.
CASE REPORT
A 63-year-old gentleman who is a known case of dyslipidemia was presented to our Emergency Department with a right sided scrotal swelling and pain for 1 week. The patient had been having right testicular pain for the past 6 months on and off but never sought medical advice. On clinical examination, the patient had right scrotal swelling with epidydimal and cord tenderness and swelling, the cremasteric reflex could not have been assessed due to the large size of the scrotum with reactive scrotal wall edema. The patient underwent Doppler ultrasound which showed right testicular heterogeneous echotexture with nodular hypo-echoic areas (Fig. 1) with preserved vascularity. There was no evidence of testicular torsion or masses in that study. A provisional clinical correlation was made and the patient was diagnosed with right epididymo-orchitis and discharged home on oral antibiotics. Next day, the patient presented again to our ER with increased pain, swelling and erythema reaching the right inguinal area. So, the patient was admitted for administration of intravenous antibiotics. After 2 days of IV antibiotics, the patient’s condition was not improving which prompted the need of a CT scan. CT scan showed a heterogeneous enlarged right testis with twisting of the spermatic cord at the level of inguinal area and scrotal neck (Fig. 2). A diagnosis of testicular torsion was made based on these findings. The patient then underwent an urgent exploration with an inguinal incision which showed a hugely edematous cord, the incision was extended as Hockey-Stick incision and the right testis was delivered. The testis was dark, edematous, with no evidence of palpable testicular masses. The spermatic cord was twisted in 1080° clockwise fashion in three areas (Fig. 3). The first 360°, torsion was at the level of the deep inguinal ring, the second at inguinal part of the spermatic cord, and the third is just proximal to the testis. Right radical orchiectomy was carried out with high ligation of the spermatic cord at the level of deep inguinal ring, which was the site of normal, non-engorged cord. The procedure was completed with the extended inguinal incision with no violation of the scrotum, since the pathology was high in the inguinal area. The patient recovered very well with no complications.
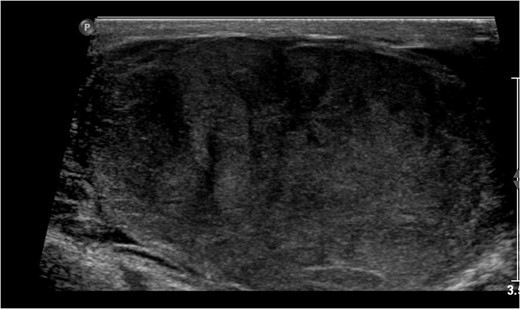
Right testicular Doppler US showing hypo-echoic areas with heterogeneous echo-texture.
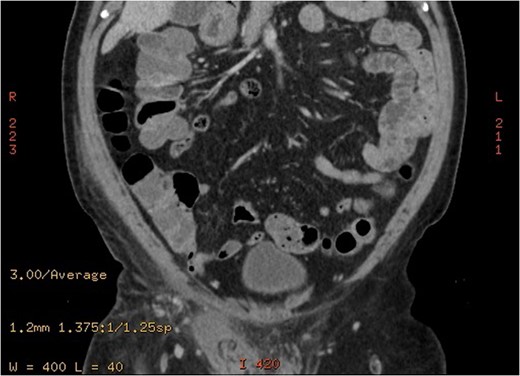
A coronal cut of and enhanced abdominal CT scan showing enlarged right spermatic cord and areas of decreased right testicular enhancement suggesting torsion.
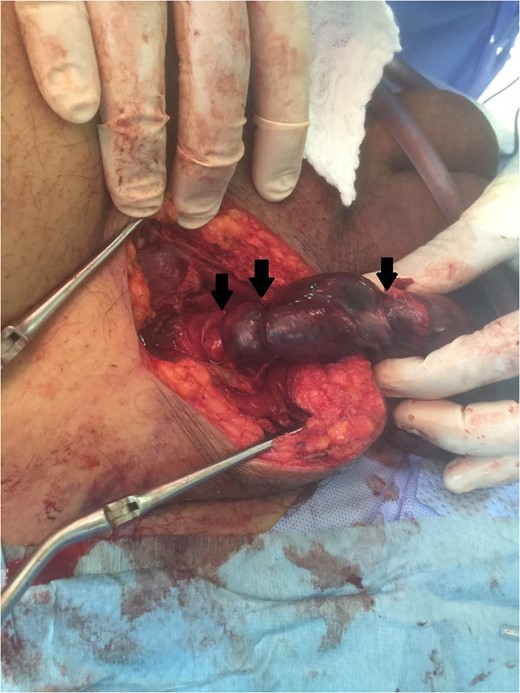
An intra-operative photo showing torsion areas (black arrows).
Surprisingly, histopathology showed a classical seminoma confined to the testis with a negative spermatic cord margin (Fig. 4). Pathology revealed a right testis that is totally hemorrhagic and necrotic with no viable tissue, a feature consistent with torsion. There are ghost of tumor infiltrate noted with morphology and imunoprofile consistent with Seminoma. Other elements of germ cell tumor and residual testis is not seen due to infarction and hemorrhage. So, the patient was worked up with a chest, abdomen and pelvis CT which showed no signs of metastasis. Tumor markers, alfa-fetoprotein, beta human chorionic gonadotropin and lactate dehydrogenase (AFP, BHCG, LDH) were taken 12 days post-operatively and were all within normal limits. Unfortunately, due to the bizarre presentation of this case, and since the initial and revised diagnoses that did not include testicular malignancy, no tumor markers were obtained preoperatively. The patient was diagnosed with stage I testicular seminoma and is being followed up now in our clinic with no evidence of local recurrence of distant metastasis.
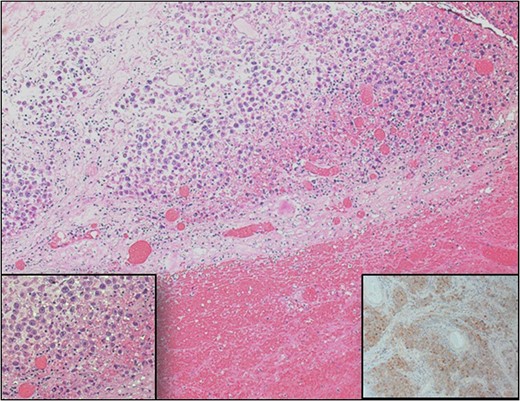
Testicular histopathology. Sections from testis show extensive hemorrhage with an area showing sheets of large round cells with clear cytoplasm. (Inset left) High power of cells show prominent nucleoli and vacuolated clear cytoplasm. (Inset right) Immunohistochemical staining of placental alkaline phosphatase (PLAP) confirms the diagnosis of classical seminoma.
DISCUSSION
Neoplasms of the testis compromise a morphologically and clinically diverse group of tumors, of which more than 95% are germ cell tumors. Germ cell tumors are relatively rare accounting for 1–2% of cancers among men in the United States. Testicular cancer is the most common solid malignancy among men 20–40 years old. Seminoma is the most common type of germ cell tumors which occur at an older average age than non-seminoma germ cell tumors, with most cases being diagnosed between the fourth and fifth decade of life. The most common presentation of testicular cancer is a painless testicular mass, while acute testicular pain is less commonly seen [6]. Diagnostic delay is a very well recognized phenomenon in literature with previous studies reporting up to one third of testicular tumors were initially misdiagnosed as epididymitis or hydrocele [7]. Intra-scrotal testicular tumor torsion is extremely rare especially in old age [2]. To our knowledge only six cases in the English literature have been reported to date [Table 1]. In our case a testicular seminoma was overlooked initially due to multiple reasons. The seminoma has a non-specific ultrasound appearance as homogeneous hypo-echoic lesions [6]. In our case this could have had been masked by the following: the presence of a testicular heterogeneous echo-texture along with nodular hypoechoic regions in testicular ultrasound going more with chronic epididymo-orchitis when correlated with long standing history of the patient, false clinical examination as the testis could not have been palpated properly due to severe edema and congestion which could have masked the firm feeling of a seminoma; the presence of severely engorged spermatic cord with patent vascularity which makes engorgement of the testis and cord more of an inflammatory process rather than torsion or malignancy.
| Case no. . | Year . | Study . | Patient age . | Location . | Pathology . |
|---|---|---|---|---|---|
| 1 | 1943 | Mohardt [8] | 26 | R | Embryonal carcinoma |
| 2 | 1983 | Cos et al. [9] | 28 | R | Seminoma |
| 3 | 1983 | Cos et al. [9] | 19 | R | Teratocarcinoma |
| 4 | 1990 | Perez [10] | 18 | L | Mixed germ cell tumour |
| 5 | 1993 | Seaman et al. [11] | 52 | L | Seminoma |
| 6 | 2011 | Gondo et al. [12] | 26 | L | Seminoma |
| 7 | 2016 | Present case | 63 | R | Seminoma |
| Case no. . | Year . | Study . | Patient age . | Location . | Pathology . |
|---|---|---|---|---|---|
| 1 | 1943 | Mohardt [8] | 26 | R | Embryonal carcinoma |
| 2 | 1983 | Cos et al. [9] | 28 | R | Seminoma |
| 3 | 1983 | Cos et al. [9] | 19 | R | Teratocarcinoma |
| 4 | 1990 | Perez [10] | 18 | L | Mixed germ cell tumour |
| 5 | 1993 | Seaman et al. [11] | 52 | L | Seminoma |
| 6 | 2011 | Gondo et al. [12] | 26 | L | Seminoma |
| 7 | 2016 | Present case | 63 | R | Seminoma |
| Case no. . | Year . | Study . | Patient age . | Location . | Pathology . |
|---|---|---|---|---|---|
| 1 | 1943 | Mohardt [8] | 26 | R | Embryonal carcinoma |
| 2 | 1983 | Cos et al. [9] | 28 | R | Seminoma |
| 3 | 1983 | Cos et al. [9] | 19 | R | Teratocarcinoma |
| 4 | 1990 | Perez [10] | 18 | L | Mixed germ cell tumour |
| 5 | 1993 | Seaman et al. [11] | 52 | L | Seminoma |
| 6 | 2011 | Gondo et al. [12] | 26 | L | Seminoma |
| 7 | 2016 | Present case | 63 | R | Seminoma |
| Case no. . | Year . | Study . | Patient age . | Location . | Pathology . |
|---|---|---|---|---|---|
| 1 | 1943 | Mohardt [8] | 26 | R | Embryonal carcinoma |
| 2 | 1983 | Cos et al. [9] | 28 | R | Seminoma |
| 3 | 1983 | Cos et al. [9] | 19 | R | Teratocarcinoma |
| 4 | 1990 | Perez [10] | 18 | L | Mixed germ cell tumour |
| 5 | 1993 | Seaman et al. [11] | 52 | L | Seminoma |
| 6 | 2011 | Gondo et al. [12] | 26 | L | Seminoma |
| 7 | 2016 | Present case | 63 | R | Seminoma |
In conclusion, Intra-scrotal testicular torsion of a seminoma is extremely rare thus Urologists should be aware of the possibility of testicular torsion being a presentation of malignancy especially in elderly. Furthermore, there is no established evidence yet supporting the etiology of torsion to be a testicular malignancy and vice versa. In a large retrospective case series done between 2003 and 2015 the association between testicular torsion and malignancy was found to be 6.4%, no etiological or histological evidence could be established rather than to describe it as an incidental finding [13]. Radiological evaluation could mask the diagnosis of malignancy especially with large edematous cord and testes. Tumor markers are helpful in such cases, however, they should not be used alone to diagnose or rule out testicular cancer, since only 10–15% of seminomas secreted B-HCG.
CONFLICT OF INTEREST STATEMENT
None declared.



