-
PDF
- Split View
-
Views
-
Cite
Cite
Sarah He, Irony Sade, Gary Lombardo, Kartik Prabhakaran, Acute presentation of congenital diaphragmatic hernia requiring damage control laparotomy in an adult patient, Journal of Surgical Case Reports, Volume 2017, Issue 7, July 2017, rjx144, https://doi.org/10.1093/jscr/rjx144
Close - Share Icon Share
Abstract
Congenital diaphragmatic hernias constitute an infrequent but potentially serious presentation of bowel obstruction in the adult patient. Herein, we present a rare case of an adult patient with strangulation of colon within a Morgagni’s hernia where timely recognition and intervention were life-saving. An 18-year-old female presented with an acute abdomen, respiratory failure, and shock secondary to a strangulated, previously undiagnosed Morgagni hernia requiring emergency laparotomy, reduction of hernia contents and resection of non-viable colon. The patient underwent repair of the hernia with restoration of bowel continuity and reconstruction of her abdominal wall in sequential fashion. Although congenital diaphragmatic hernias have been previously described in the adult population, there are few if any reports of such pathology presenting in such an acute, life-threatening fashion. This case highlights the importance of a high index of suspicion, early recognition, and timely surgical intervention for this rare, potentially fatal condition.
INTRODUCTION
Diaphragmatic hernia, congenital or acquired, is a herniation of abdominal contents into the thoracic cavity due to a defect in the diaphragm. Congenital diaphragmatic hernias (CDH) are comprised of posterolateral (Bochdalek) hernias (most common), anterior-retrosternal (Morgagni) hernias (rarest), hiatal hernias and septum transversum defects. Morgagni’s hernia results from the failure of closure of the pars sternalis leading to an anterior medial septum transversum defect [1]. Presentations in the pediatric population are more commonly acute, and frequently present as recurrent chest infections. In adults, chronic pain and pulmonary complaints are the most common presentations of a Morgagni hernia [2]. Rarely do patients present acutely with gastric volvulus or bowel obstruction [3]. The average reported age of presentation amongst adult patients is >50 years old.
It is widely accepted that both symptomatic and asymptomatic patients should undergo surgical repair [1]. However, since the true prevalence of Morgagni hernias has not been reported, it is impossible to compare operative and non-operative management and determine the benefit of either approach [3]. While presentation and repair of Morgagni’s hernia has been described in the adult population, we describe in this report a unique case in which a previously undiagnosed Morgagni’s hernia presented in the form of an acute abdomen, respiratory failure and septic shock owing to strangulated hollow viscera.
CASE REPORT
An 18-year-old otherwise healthy female patient presented to a local community hospital emergency department with a 3-day history of non-specific abdominal pain. While at the referring facility, the patients’ pain progressed rapidly to peritonitis. Initial evaluation at the referring facility included a CT scan, which demonstrated herniated large bowel into her thoracic cavity through a suspected anterior/retrosternal hernia (Fig. 1). The patient was transferred to our institution for further management.

Coronal view of herniated colon on computed tomography scan obtained at the referring facility prior to transfer.
Upon arrival to our emergency department, the patient was febrile, obtunded and with a heart rate of 200 beats per minute. Her abdominal exam was consistent with peritonitis and her laboratory studies were consistent with shock and lactic acidosis. During evaluation by the surgical team, the patient required emergent intubation for progressive respiratory distress with ongoing fluid resuscitation for the treatment of shock. En route to the operating suite, the patient demonstrated rapid escalation in airway pressures, and cardiac arrest. After return of spontaneous circulation, a post-intubation chest radiograph demonstrated opacification of her left thoracic cavity and a coiled nasogastric tube within her stomach above her diaphragm (Fig. 2). Her abdomen became progressively more distended, concerning for abdominal compartment syndrome. With ongoing bag-mask ventilation, the patient was rushed to the operating room for emergent laparotomy.
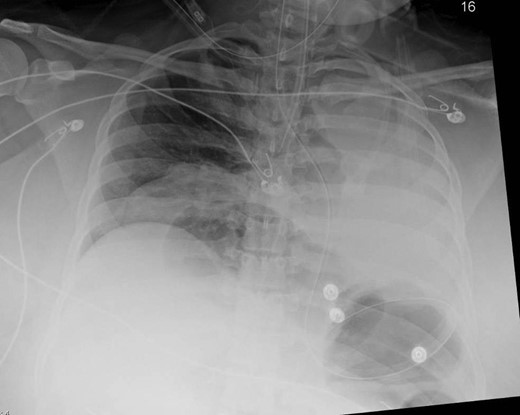
Anterior–posterior chest x-ray obtained after intubation demonstrating bowel loops and a coiled nasogastric tube within the stomach, above the diaphragm and a coiled nasogastric tube above the diaphragm.
Laparotomy revealed intra-abdominal contents under pressure with turbid fluid. Manual reduction of the retrosternal diaphragmatic hernia contents revealed strangulated ascending and transverse colon with full thickness necrosis and an incarcerated yet viable stomach. The contents of the hernia (stomach, ascending and transverse colon) were carefully reduced and a 3 × 3 cm2 hernia defect was noted in the retrosternal position which was repaired primarily. The hernia sac was reduced and excised. An extended right hemicolectomy was performed in damage control fashion, leaving the bowel in discontinuity with a plan for re-exploration after further resuscitation.
Thereafter, the patient was admitted to the ICU for further resuscitation. She was gradually weaned off vasopressors, and sedation was weaned revealing intact neurologic function. After normalization of her physiologic parameters, the patient was taken back to the operating room for planned re-exploration at which time a gastrostomy tube was placed, and further necrotic bowel margins were resected. She subsequently underwent two additional planned abdominal re-explorations resulting in restoration of intestinal continuity with an ileo-descending colon anastomosis and reconstruction of her abdominal wall utilizing a biologic mesh. Due to prolonged ventilator dependency and respiratory failure, a tracheostomy was performed on hospital Day 10. Her post-operative course was unremarkable and she was downgraded from the ICU on hospital Day 23, decannulated on Day 30, and was discharged on hospital Day 33 after tolerating a regular diet. She suffered no neurologic sequelae and has since resumed full activities of daily living.
DISCUSSION
In the adult population, the presence of a congenital diaphragmatic hernia is approximately one in 133 000 and is often associated with presentation in later years of life [2]. A large percentage of patients are asymptomatic or present with very non-specific gastrointestinal or respiratory signs and symptoms [4]. Rarely does a Morgagni hernia present acutely; in a recent literature review only 13% of adults presented with less than a week of symptoms whereas most commonly patients had non-specific symptoms for up to 6 months [2].
Once discovered, it is widely accepted that both symptomatic and asymptomatic patients should undergo surgical repair [1]. Options for repair include transthoracic, transabdominal or laparoscopic approaches. The transabdominal approach allows easier reduction of the hernia and the viscera can be pulled down into the abdomen [2] where a ventral hernia can be left if the contents do not fit. This approach is mandatory when complications such as strangulation or perforation with peritonitis are present.
The case presented herein highlights an unusual presentation of a congenital diaphragmatic hernia. Despite her youth, lack of comorbidities, and acute nature of her presentation, our patient had decompensated precipitously from strangulation of her colon, producing profound physiologic sequelae of septic shock. The development of abdominal compartment syndrome and hemodynamic instability mandated a damage control approach to the patient in which resection of non-viable bowel and abdominal decompression were prioritized. Despite a history of normal development, the question remains as to whether there were any historical signs or symptoms during the patient’s childhood that could have portended such an acute presentation. More importantly, the age of the patient when combined with the radiographic findings should raise a high index of suspicion for a congenital defect with profound potential consequences if left untreated. Given the small size of the defect when compared to parasesophageal hernias, the risk of strangulation of viscera is much greater, and should lead the clinician to act immediately upon confirmed diagnosis.
CONFLICT OF INTEREST STATEMENT
None declared.
References
- acute abdomen
- adult
- hernias
- intestinal obstruction
- intestines
- laparotomy
- reconstructive surgical procedures
- respiratory insufficiency
- shock
- surgical procedures, operative
- colon
- pathology
- abdominal wall
- hernia of foramen of morgagni, congenital
- hernia, congenital diaphragmatic
- strangulation
- undiagnosed



