-
PDF
- Split View
-
Views
-
Cite
Cite
Saqib Saeed, Ofikwu Godwin, Albert K. Adu, Alexius Ramcharan, Pneumomediastinum and subcutaneous emphysema after successful laparoscopic supra-cervical hysterectomy, Journal of Surgical Case Reports, Volume 2017, Issue 7, July 2017, rjx146, https://doi.org/10.1093/jscr/rjx146
Close - Share Icon Share
Abstract
Laparoscopic hysterectomy is a commonly performed gynecological procedure. Although the outcomes are favorable, severe life threatening complications such as pneumothorax, pneumomediastinum and subcutaneous emphysema can occur during laparoscopy secondary to carbon dioxide insufflation. We report a 46-year-old female who was scheduled for laparoscopic-assisted supra-cervical hysterectomy for uterine fibroids. Patient tolerated the procedure and there were no intra-operative complications. Post operatively she developed hypercarbia, subcutaneous emphysema and pneumomediastinum. She was managed conservatively. This case demonstrates a rare occurrence of subcutaneous emphysema and pneumomediastinum after supra-cervical hysterectomy.
INTRODUCTION
Laparoscopic hysterectomy (LH) is the standard of care for almost all benign gynecological conditions. According to the Department of Health and Human Services, 600 000 hysterectomies are performed in the US every year [1, 2], and one-third of American women will have the procedure by the time they turn 60. Although the complications are usually minor and patients may return to their usual activities in a day or 2, severe and serious complications such as pneumomediastinum can arise, necessitating the intervention of both the gynecologist and general surgeon, resulting in prolonged hospital stay and cost of care [3]. We present a case of a 46-year-old female who developed pneumomediastinum and subcutaneous emphysema following laparoscopic supra-cervical hysterectomy and bilateral salpingo-oophorectomy for uterine fibroids.
CASE REPORT
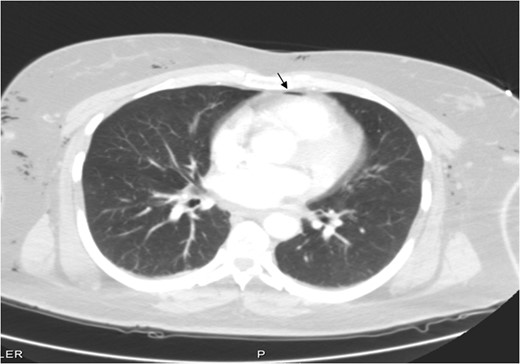
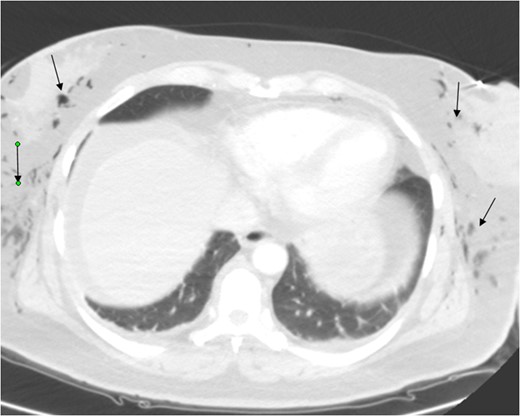
A 46-year-old female, Gravida 3 para 3, all alive, with past medical history of depression, acid reflux and uterine fibroids presented to our emergency unit with acute exacerbation of lower abdominal pain, vaginal bleeding and dizziness, which she had for a month. On examination, her abdomen was soft, with tenderness to right and left lower quadrants. Pelvic examination showed a 14-week uterus, per vaginal bleed and closed cervical os. A repeat sonogram showed the uterus to be 13.9 × 4.8 × 7.1 cm3 with three dominant intramural fibroids. Fundal fibroid measured 3.3 cm, mid posterior uterine fibroid measured 2.2 cm and mid/lower uterine fibroid, 3.8 cm. The central endometrial echo was normal. The right ovary measured ~2.5 × 1.7 × 3.0 cm3 while the left ovary, was 2.5 × 1.9 × 1.7 cm3. Her hematocrit and hemoglobin on presentation were 32% and 11 g/dl, respectively, down from 42% and 14 g/dl a week earlier. She was scheduled for laparoscopic-assisted vaginal supra-cevical hysterectomy with bilateral salpingo-oophorectomy. The operative technique required placing the patient in steep Trendelenburg position and use of a Veress needle through an umbilical incision for insufflation of 3 l of carbon dioxide at a pressure of 15–20 mmHg. All trocal placements were done without complications. Estimated blood loss was 700 ml. The operative time was 7 h (420 min). Surgery was complicated with carbon dioxide overload and retention, with partial pressure of carbon dioxide (PCO2) of 67 mm of mercury (mmHg) immediately post operatively. Patient developed extensive subcutaneous emphysema, and pneumomediastinum (Figs 1–3) on first post-operative Day 1, requiring intubation and mechanical ventilation. Her minute ventilation was increased to wash off the excess CO2. She was sedated and managed expectantly with observation and watchful waiting in the intensive unit. Both subcutaneous emphysema and pneumomediastinum resolved spontaneously by post-operative Day 3 with non-operative treatment. She was eventually discharged in stable condition on post-operative Day 3 and followed up in clinic with no residual issues.
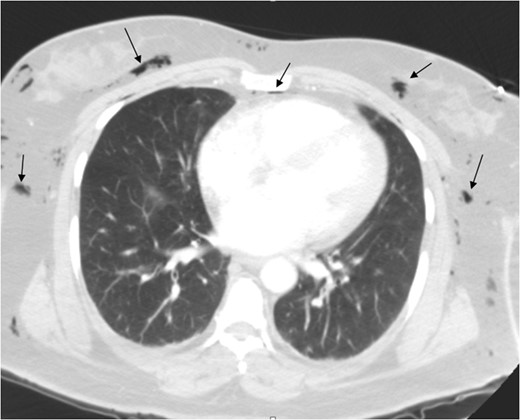
Pneumomediastinum and subcutaneous emphysema as indicated by the arrows.
DISCUSSION
Hysterectomy can be performed for benign and malignant indications. Approximately 90% of hysterectomies are performed for benign conditions, such as fibroids resulting in abnormal uterine bleeding [4]. The lifetime risk of a woman having to undergo hysterectomy because of a benign disorder is 30% in the United States. There are three main approaches to hysterectomy performed for benign indications: abdominal hysterectomy (AH), vaginal hysterectomy (VH) and LH [5]. Compared to AH, VH is regarded as less invasive and seemed to have the advantages of lower morbidity and lower risk of injury to the ureter. Over the last two decades, the proportion of hysterectomies performed by LH has gradually increased. Although the surgery tends to take longer, it has numerous advantages over the AH, including quicker return to normal activities, less blood loss and a shorter hospital stay, fewer wound complications compared to AH [6].
There are three subcategories of LH. First, LH where the uterine vessels are ligated laparoscopically but part of the operation is performed vaginally. Secondly, laparoscopic-assisted VH (LAVH), where the laparoscopic component of the procedure does not involve division of the uterine vessels; and lastly, total LH (TLH), where the entire procedure including suturing of the vaginal vault is performed laparoscopically. Our patient had LAVH. Some of the complications associated with laparoscopic approach are subcutaneous emphysema, hypercarbia, pneumothorax and or pneumomediastinum.
Murdock et al. [7] found incidence rates of 5.5% for hypercarbia, 2.3% for subcutaneous emphysema, and 1.9% for pneumothorax/pneumomediastinum following laparoscopic approach. Predictors of the development of subcutaneous emphysema, were maximum positive end-tidal CO2 (PETCO2), >50 mmHg, operative time >200 min, and the use of six or more surgical ports. Variables that predicted the development of pneumothorax and/or pneumomediastinum, were PETCO2 > 50 mmHg and operative time >200 min. Cardiovascular changes and significant respiratory acidosis have been observed in otherwise healthy patients during laparoscopic procedures [8].
Hypercarbia is the most commonly recognized respiratory complication. A combination of factors contribute to the increased arterial PaCO2. Reduced diaphragmatic movement, a decrease in residual functional capacity, and decreased pulmonary CO2 excretion lead to ventilation–perfusion mismatching. Another factor that may increase CO2 level is subcutaneous emphysema with absorption [9].
Dissection of the insufflated CO2 from the peritoneal cavity to the subcutaneous tissue may occur at the trocar site or via a defect in the diaphragm. Intra-abdominal pressure of CO2 should therefore be monitored, since high pressures are associated with a higher incidence of subcutaneous emphysema. Following CO2 absorption into the blood, the gas is stored in visceral and muscle tissue, delaying prompt elimination via the lungs.
Our patient developed hypercarbia, PCO2 of 67.9 mmHg immediately post operatively and was noted to have developed subcutaneous emphysema and pneumomediastinum on first post-operative Day 1. Hypercarbia was treated by increasing her minute ventilation to wash off the excess CO2. Both subcutaneous emphysema and pneumomediastinum resolved spontaneously with observation and watchful waiting in the intensive unit. This is in line with Successful Non-surgical Treatment of Pneumomediastinum, Pneumothorax, Pneumoperitoneum, Pneumoretroperitoneum and Subcutaneous Emphysema described by Fugii et al. [10]
In conclusion, gynecological surgeons should always be aware of the possibility of development of serious complications like pneumomediastinum during or immediately after LH. Outcomes are favorable with conservative Management.
CONFLICT OF INTEREST STATEMENT
None declared.



