-
PDF
- Split View
-
Views
-
Cite
Cite
Masahiro Shiihara, Takaaki Kato, Yuka Kaneko, Kenji Yoshitoshi, Takehiro Ota, de Garengeot hernia with appendicitis treated by two-way-approach surgery: a case report, Journal of Surgical Case Reports, Volume 2017, Issue 7, July 2017, rjx140, https://doi.org/10.1093/jscr/rjx140
Close - Share Icon Share
Abstract
de Garengeot hernia is a rare subtype of a femoral hernia with incarceration of the appendix. This type of hernia usually presents with therapeutic dilemmas, especially because of the risk of surgical site infection (SSI). Our patient was a 74-year-old woman with a bulging mass and tenderness in the right inguinal area. Computed tomography revealed an incarcerated appendix, with appendicitis in the femoral hernia. Laparoscopic appendectomy was initially performed, followed by hernioplasty via the anterior approach to prevent properitoneal contamination. Some authors have recently reported cases successfully treated by laparoscopy. However, this type of hernia has a higher risk for SSI, compared with the risk involved in usual hernioplasty. Therefore, selection of the appropriate surgical approach to prevent wound infection is important, especially in the presence of appendicitis. We would like to highlight the usefulness of hybrid surgery, laparoscopic appendectomy and hernioplasty via the anterior approach to prevent SSIs.
INTRODUCTION
de Garengeot hernia is described as femoral hernia containing the appendix. It was first reported in 1731 by the French surgeon Rene Jacques Croissant de Garengeot. This rare condition occurs in 0.49% of femoral hernias [1]. The presence of acute appendicitis within a de Garengeot hernia is rarer, with an incidence of 0.08–0.13% [2]. To our knowledge, fewer than 100 cases of de Garengeot hernia have been reported, and no standard surgical approach has been described for this condition. We recently found some cases that were successfully treated using the laparoscopic approach, in the literature. However, the treatment for this condition along with acute appendicitis is still controversial. We present a case of a patient with de Garengeot hernia with appendicitis who was successfully treated by performing a hybrid surgery, laparoscopic appendectomy, and anterior hernioplasty.
CASE REPORT
A 74-year-old woman with aplastic anaemia and hypertension who complained of a bulging mass and tenderness in the right inguinal area was referred to our department. She was afebrile, normotensive, and denied abdominal pain, bloating, nausea or vomiting. Upon physical examination, a swelling mass measuring 3 cm × 3 cm was observed just below the right inguinal ligament. The swelling was irreducible but not strangulated. Laboratory examination findings showed that the white blood cell count and C-reactive protein level of the patient were within the normal range, but the percentage of neutrophilic leucocytes was slightly increased, at 73.7%. Abdominal enhanced computed tomography (CT) revealed a swelling and an enhanced appendix within the femoral hernia (Fig. 1). Hence, a diagnosis of de Garengeot hernia with suspected acute appendicitis was made, and surgery was performed. A 12-mm trocar was inserted under the umbilicus, and a 30° laparoscope was used to examine the abdominal cavity. No ascites or dilated bowels were observed. The major part of the appendix passed through the femoral orifice (Fig. 2). Then, two additional 5-mm trocars were inserted in the left lower and middle abdominal regions. The hernia could be reduced by deliberately pulling the appendix. A necrotic and inflamed appendix was detected (Fig. 3a). Subsequently, laparoscopic appendectomy was performed. Hernioplasty was performed via the anterior approach to prevent properitoneal contamination. The hernial defect was repaired using a mesh plug. The incarcerated hernia sac was reduced via the extraperitoneum, and it was then ligated and resected via laparoscopy (Fig. 3b). The pathological findings showed acute purulent appendicitis. The postoperative course of the patient was uneventful, without any surgical site infection (SSI), and she was discharged on the postoperative Day 8.
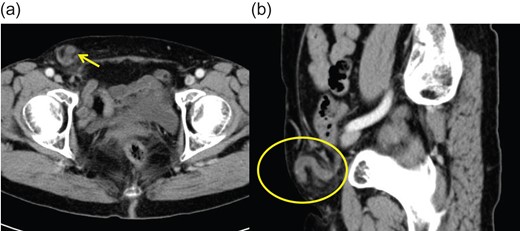
Abdominal enhanced computed tomography imaging showing (a) the enhanced tubular structure in the femoral hernia and (b) the caecum.
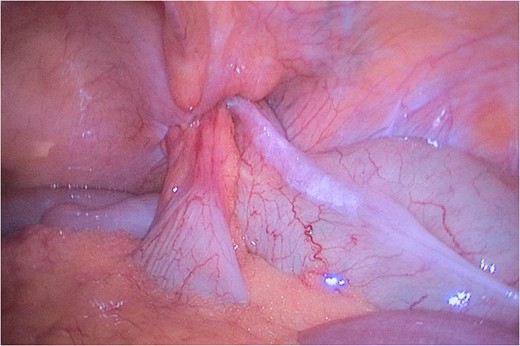
Laparoscopic findings showing migration of the appendix into the femoral hernia.
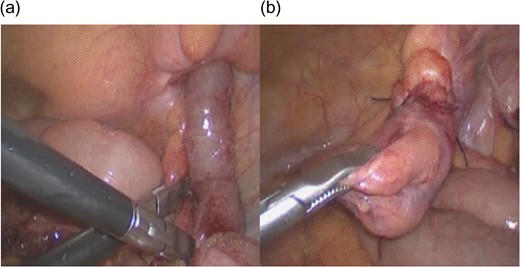
(a) Inflamed and partly necrotic appendix was reduced during laparoscopy. (b) Hernial sac was ligated and cut during laparoscopy.
DISCUSSION
de Garengeot hernia is defined as a femoral hernia containing the appendix. It is a rare condition that presents with a swelling mass in the groin, which is often tender. Femoral hernia is more common in women, especially in postmenopausal women. It has higher risks for incarceration and strangulation, which are estimated to be 20 and 45% at 3 and 21 months, respectively, compared to inguinal hernia, whose risks for incarceration and strangulation are estimated to be 3 and 4.5% at 3 and 21 months, respectively [3]. Thus, early surgery is often required.
Some theories have proposed the pathogenesis of the migration of the appendix into the femoral hernia. One theory is abnormal intestinal rotation during embryological development, and appendiceal attachment is another theory. A mobile caecum, large caecum or visceroptosis is also considered a risk factor for de Garengeot hernia [1, 4]. In our patient, the caecum was fixed at a lower position.
The preoperative diagnosis of de Garengeot hernia was known to be difficult. However, a preoperative diagnosis has often been reported in recent studies, mostly through CT [5]. CT demonstrates a tubular structure following the caecum in the femoral hernia.
Surgical management of de Garengeot hernia is controversial. Several surgical approaches exist, including open or laparoscopic approaches either with or without appendectomy, with mesh or simple suture hernioplasty. We found some recent reports on cases in which the patients were successfully treated using the laparoscopic approach [6]. Some authors reported that transabdominal preperitoneal hernioplasty had the benefit of diagnostic laparoscopy, and they could concurrently perform appendectomy. However, in patients with appendicitis, the risk of mesh infection should be prevented. The rate of SSI for inguinal and femoral hernia repairs is 0.45% (352/77 666) [7]. Moreover, the rates of SSI are 6.7 and 3.3% for open and laparoscopic appendectomy, respectively [8]. However, the rate of SSI following procedures involving bowel obstruction/necrosis was higher than that after procedures without obstruction/necrosis for hernia repair (0.89 vs. 0.44%, P < 0.001). Sharma et al. [9] reported that one of their three patients with de Garengeot hernia developed wound infection after infra-inguinal incision was performed during appendectomy and hernioplasty. In our case, laparoscopic findings revealed an inflamed and necrotic appendix. We performed appendectomy and hernioplasty via different approaches to prevent mesh contamination. Some authors recommended a simple suture repair in appendectomy [10]. Although some authors have reported successful mesh repairs per infra-inguinal incision performed in the presence of appendicitis, we insist that the surgical site of hernioplasty should not be contaminated. Thus, we recommend different incision approaches, as applied in our case, or interval hernioplasty, especially in patients with concurrent appendicitis.
CONCLUSION
Hybrid surgery, laparoscopic appendectomy and hernioplasty via the anterior approach are recommended in patients with de Garengeot hernia with appendicitis. Using a different approach for each surgery could help prevent contamination of the surgical site.
CONFLICT OF INTEREST STATEMENT
None declared.



