-
PDF
- Split View
-
Views
-
Cite
Cite
Lauren E. Smith, Acute GI bleed due to leiomyoma of the jejunum: a case report, Journal of Surgical Case Reports, Volume 2017, Issue 7, July 2017, rjx138, https://doi.org/10.1093/jscr/rjx138
Close - Share Icon Share
Abstract
Neoplasms of the small intestine are rare. Leiomyomas are the one of the benign neoplasms that can be found in the small intestine. These lesions usually remain asymptomatic and are often found incidentally; however, they can become symptomatic if obstruction occurs or the tumor outgrows its blood supply resulting mucosa. Their clinical manifestations can include abdominal pain, diarrhea, melena, a palpable abdominal mass and weight loss. Due to their vague presentation, leiomyomas of the small intestine are typically diagnosed after failed conservative therapy for other pathologies such as duodenal ulcers and diverticulosis. This case report describes a 34-year-old male who developed an acute GI bleed due to a symptomatic leiomyoma of the jejunum. He was initially treated with non-operative conservative management; however, his symptoms remained unresolved and he went on to require surgical intervention.
INTRODUCTION
Neoplasms of the small intestine are rare. Leiomyomas are one of the benign neoplasms that can be found in the small intestine. These lesions usually remain asymptomatic and are often found incidentally; however, they rarely can become symptomatic if obstruction occurs or the tumor outgrows its blood supply. Few case reports of symptomatic jejunal leiomyomas have been documented in the literature. This case report describes a 34-year-old male who developed an acute GI bleed due to a leiomyoma of the jejunum.
CASE REPORT
A 34-year-old male presented to the ER complaining of lower abdominal pain and rectal bleeding of 6 days duration. He stated that he had been having dark, maroon-colored stools three or four times daily. There were no prior episodes of hemorrhage. He admitted to dizziness and fatigue; however, he denied any fever, chills, nausea, vomiting, chest pain or shortness of breath. His past medical history was significant for one episode of diverticulitis ~7 years prior. He denied any previous history of endoscopy or abdominal surgeries. His family history was positive for hypertension. Socially, he was married and admitted to occasionally smoking cigars. He denied taking any medications regularly.
On physical exam, he was noted to be afebrile, normotensive and mildly tachycardic. The abdomen was soft with tenderness to palpation in the left lower quadrant. There were normoactive bowel sounds. Dark colored blood was noted perianally on rectal exam. Laboratory data demonstrated leukocytosis of 14 800, a hemoglobin of 8, and a hematocrit of 23.9%. Renal function, electrolytes and urinalysis were all within normal ranges.
A CT of the abdomen and pelvis without contrast was obtained on admission and revealed a 7 × 7.6 cm2 mass with CT attenuation of 37.34 Hounsfield units within the anterior left midpelvis. It appeared to be inseparable along its superior aspect from a loop of bowel, and it was felt to possibly be an unusual diverticulum. The patient was given intravenous fluids and one unit of packed red blood cells for his symptomatic anemia with continued rectal bleeding. He was also empirically started on Cipro and Flagyl for possible infection coverage. GI was consulted and the patient was taken for an EGD and colonoscopy; however, both were negative for any acute pathology.
General surgery was then consulted for further recommendations. A CT of the abdomen and pelvis with contrast was performed and demonstrated a 7.2 × 6.8 × 6.1 cm3 lesion arising from the mid-to-distal small bowel loop with no evidence of significant enhancement. It appeared mobile within the mesentery of the small bowel when compared to previous imaging (Figs. 1 and 2). The patient had continued to bleed and required transfusion with five units of packed red blood cells; therefore, it was decided to take the patient to the operating room for a diagnostic laparoscopy.
Once in the abdomen, a large, pedunculated mass within the wall of the small bowel was noted in the right lower quadrant. The mass was highly vascular appearing (Fig. 3). At this point, the procedure was converted to a mini-laparotomy and the mass was excised in its entirely. Ten centimeter margins of the small bowel were resected both proximally and distally to the mass. A primary anastomosis of the small bowel was made and the abdomen was closed in a multi-layer fashion. The patient did well post-operatively and he was discharged home 2 days after surgery.
The resected mass was sent to pathology for further evaluation. The final pathological diagnosis was leiomyoma of the jejunum. The tumor demonstrated involvement in the jejunal muscularis propria without extension into the overlying mucosa. There were no involved lymph nodes. A cut section of the mass revealed a firm, gray-white, whorled appearance. A panel of immunoperoxidase stains was performed. The tumor cells showed strong, diffuse positive staining for smooth muscle actin and desmin. All other stains, including CD34, CD117, S-100 and bcl-2, were negative. While the differential diagnosis of a spindle cell neoplasm involving the jejunum would include a gastrointestinal stromal tumor, the immunotype and morphologic features of these tumor cells were more consistent with leiomyoma. There were no malignant features identified.
The patient was seen at 2- and 4-week follow-up. He reported complete resolution of his previous symptoms. He was instructed to follow-up on an as-needed basis.
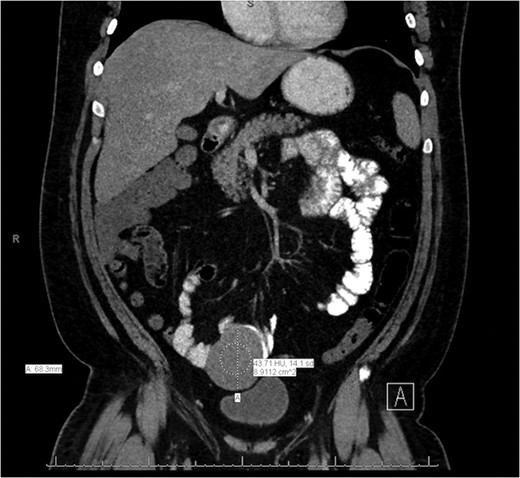
Coronal slice of the CT of the abdomen/pelvis demonstrating a lesion arising from the mid-to-distal small bowel.
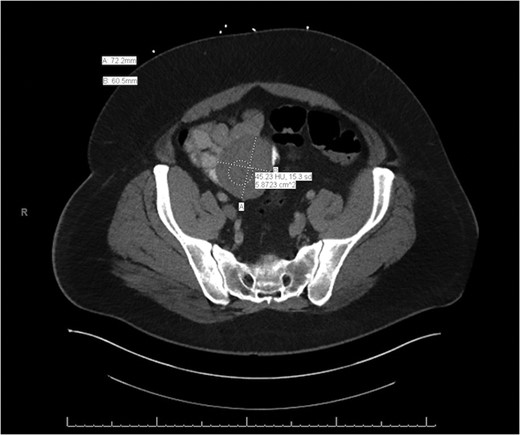
Axial slice of the CT of the abdomen/pelvis demonstrating a lesion arising from the mid-to-distal small bowel.

Intraoperative photograph of large, pedunculated mass arising from the wall of the jejunum.
DISCUSSION
The first documented evidence of a leiomyoma in the small intestine dates to 1858 [1, 2]. In 1932, 11 500 autopsy reports and 45 000 surgical specimens were examined at Johns Hopkins University Hospital. This examination revealed a total of 88 small bowel tumors, of which only three were leiomyomas [1].
These tumors are known for bleeding due to central necrosis, liquefaction and expulsion of the tumor’s contents into the lumen of the bowel [1]. Their clinical manifestations can include abdominal pain, diarrhea, melena, a palpable abdominal mass and weight loss. Not surprisingly, symptomatic leiomyomas can easily be mistaken for other pathologies such as duodenal ulcers and diverticulosis. As a result, they are frequently diagnosed after failed conservative treatment for a mistaken pathology.
Cherry et al. examined multiple cases in which the initial diagnosis of duodenal ulcer was made; however, operation or autopsy revealed that a leiomyoma was responsible for the patients’ symptoms. Because other reports also support this finding, leiomyoma of the small intestine can be considered one of the ‘great imitators’ [3–5].
While duodenal ulcers and diverticulosis are certainly more common than symptomatic neoplasms of the small intestine, it is important to have a higher index of suspicion for additional etiologies, especially when irregularities of imaging studies are noted and the patient fails initial conservative management.
ACKNOWLEDGMENTS
I would like to thank Dr Stephen Fleischer at Grandview Medical Center as well as the entire surgical staff for their assistance.
FUNDING
None.
CONFLICT OF INTEREST STATEMENT
None declared.
ETHICAL APPROVAL
Ethical approval from the Kettering Health Network institutional review board was obtained (IRB# 00001338).
CONSENT
Consent from the patient for this case report was obtained.
REFERENCES
- abdominal mass
- abdominal pain
- vascular flow
- weight reduction
- diarrhea
- duodenal ulcer
- intestine, small
- fibroid tumor
- melena
- signs and symptoms
- surgical procedures, operative
- jejunum
- mucous membrane
- neoplasms
- diverticulosis
- small intestinal neoplasms
- benign neoplasms
- vasculature
- small intestine leiomyomas
- blood supply, arterial
- conservative treatment
- acute gastrointestinal hemorrhage



