-
PDF
- Split View
-
Views
-
Cite
Cite
Tomoi Sato, Ichiro Muto, Takeshi Oya, Takeshi Sakai, Invasive Paget’s disease of the male nipple: a case report, Journal of Surgical Case Reports, Volume 2017, Issue 7, July 2017, rjx137, https://doi.org/10.1093/jscr/rjx137
Close - Share Icon Share
Abstract
Male mammary Paget’s disease (MPD) is extremely rare. Furthermore, MPD with invasion downward into the dermis of the male nipple has been reported rarely. A 56-year-old Japanese man presented with a lump and eczema in the right nipple–areola area. Ultrasonography revealed only a cystic lesion below the right areola. With a diagnosis of MPD with invasion into the dermis associated with ductal carcinoma in situ, mastectomy and sentinel lymph node biopsy were performed. MPD with dermal invasion is extremely rare, and only one male case has been reported in the English literature; therefore, the current case is the second case of male MPD with dermal invasion.
INTRODUCTION
Female mammary Paget’s disease (MPD) is relatively uncommon, but male MPD is so rare that only a few case reports exist [1]. Although most MPDs are in situ carcinoma spreading within the epidermis of the nipple–areolar complex, on rare occasions Paget’s cells can infiltrate downward into the dermis [2–6]. We report here an extremely rare case of MPD with direct invasion into the dermis in a Japanese man.
CASE REPORT
A 56-year-old Japanese man presented with eczema and redness of the right nipple (Fig. 1) and an 11 mm lump located in the right sub-areolar area. He had no notable familial history, and had no medical history except surgery for a cerebral hemorrhage 2 weeks previously. Ultrasound revealed a cystic mass below the right areola (Fig. 2), but no obvious invasive tumor. Skin biopsy of the nipple eczema revealed Paget's cells in the epidermis and possible invasive foci infiltrating the underlying dermis. Computed tomography revealed only a cystic mass in the right breast and no distant metastasis.

Right breast after skin biopsy. Erosion and redness of the nipple–areola complex were noted. A lump, 11 mm, was palpated in the breast. A skin biopsy suture can be seen.
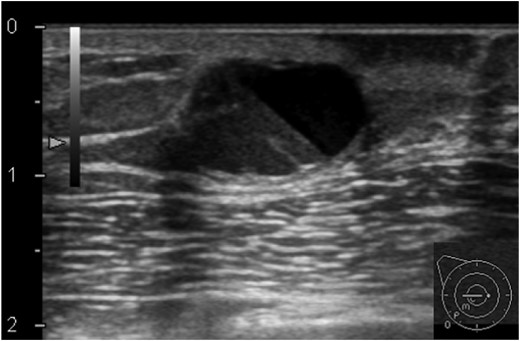
Ultrasonography of the right breast at first presentation. A cystic mass, 13 mm, with the appearance of rippling water can be seen below the right areola.
The patient underwent right mastectomy and sentinel lymph node biopsy (SLNB). Histologically, ductal carcinoma in situ (DCIS) in the cystic lesion of the right breast parenchyma (16 × 14 × 14 mm3, Fig. 3A and B) and MPD (26 × 16 mm2) were found, both of which were connected via intraductal spread in the major lactiferous duct (Fig. 3C). Paget’s cells directly infiltrated the dermis, with an invasive focus of 15 mm in the largest diameter and 2.5 mm in depth from the dermoepidermal junction (Fig. 3D–F). Immunohistochemistry revealed strongly positive staining for estrogen receptor (ER, Fig. 3F) in most cells (>90%), moderately for progesterone receptor (PgR) in some cells (20%), partly for cytokeratin (CK)-7, and CAM5.2 (Fig. 3E) but negative for Her2, S-100, HMB-45 and CK-5/6. The Ki67 labeling index of the invasive focus was 15%. The sentinel node was free from metastasis.
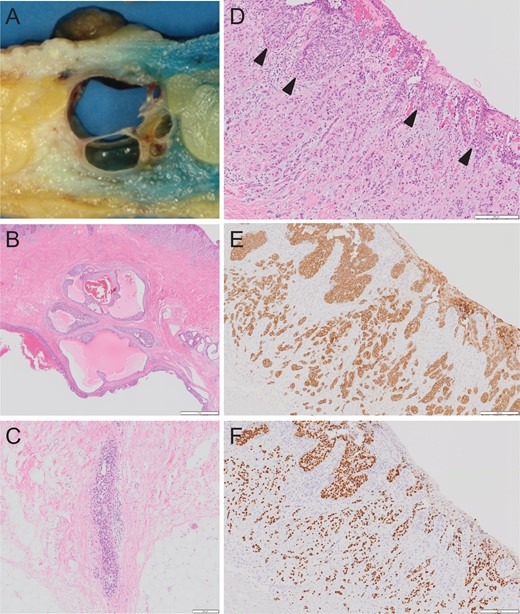
Macroscopic appearance of the specimen (A). Multiple cystic lesions can be seen below the nipple. Histopathological findings of non-invasive breast cancer in the cystic lesion of the breast parenchyma (B). Ductal carcinoma cells can be seen. Intraductal spread in the major lactiferous duct (C). Histopathological findings of Paget’s cells (arrowhead) and invasive foci in the dermis (D). Immunohistochemical study of the Paget’s cells and invasive foci revealed diffusely positive staining for CAM5.2 (E) and ER (F).
The patient has been doing well with tamoxifen for 38 months.
DISCUSSION
Male BC is rare, representing <1% of all breast cancers. MPD is also uncommon and accounts for ~1% of all breast malignancies. Thus, male MPD is extremely rare, and only a few case reports exist. Adams et al. [1] summarized 24 cases of male MPD published since 1997. In SEER Data during 1973–2012, there were only 120 (1.45%) cases of male MPD out of 8295 cases of male BC [1].
MPD is usually characterized by malignant glandular cells with clear cytoplasm and eccentric, hyperchromatic nuclei within the epidermis, and thus, is considered to be in situ BC; however, MPD with dermal invasion can occur [2–6]. Lee et al. [2] reported 16 invasive cases out of 205 cases of MPD (7.8%) during 1994–2013. In addition, they summarized 31 cases of invasive MPD with an additional 15 reported cases. Of these, only one male invasive case of MPD was reported by Chao et al. [3]; therefore, the current case is the second case of male MPD with dermal invasion.
The differential diagnosis includes psoriasis, contact dermatitis, erosive adenomatosis of the nipple, intraductal papilloma, nipple adenoma, basal cell carcinoma, Bowen’s disease (intraepithelial squamous cell carcinoma), malignant melanoma, and Toker cell hyperplasia [1]. In the present case, the diagnosis of MPD could be made via pathological findings with underlying DCIS. Immunohistochemical study further supported its origin in the breast. If differentiation between MPD and melanoma is unreliable, immunohistochemical study for melanocytes such as HMB-45 or S-100 is helpful [1]. The staining pattern of CK-7, CK-5/6 and CAM5.2 is inverse in MPD and Bowen’s disease [1].
In addition, it is important to distinguish invasive MPD from the following conditions because their treatments and prognoses are completely different: underlying invasive BC directly infiltrates upward into the dermis and spreads in the epidermis; satellite skin nodule from invasive BC. In the current case, the absence of invasive BC in the breast parenchyma, the continuity of underlying DCIS and Paget’s disease via ductal spread of the major lactiferous duct, and infiltration of the same Paget’s cells into those in the overlying epidermis indicate that MPD had invaded downward into the underlying dermis.
In the treatment of MPD, surgical management is primarily required. Modified radical mastectomy or simple mastectomy has been performed in most cases of male MPD [1]. Sukumvanich et al. [7] reported that among MPD without clinical findings of underlying BC, invasive BC was found in 27% of patients and 11% had SLN metastases [7]. Some authors have reported cases of invasive MPD with underlying DCIS which had axillary lymph node metastasis [4, 5]; therefore, even if obvious invasive BC is absent in the breast parenchyma, SLNB should be considered in clinical node-negative MPD.
The impact of invasive MPD on the prognosis remains to be elucidated. Usually, the prognosis of MPD depends on an underlying BC, which is frequently associated with MPD [2]. Lee et al. [2] determined the clinical outcome between invasive MPD and matched non-invasive MPD as a control. The results showed no differences in prognosis, probably because the depth of invasion was up to 2 mm in all cases, and the size of invasive foci was up to 1 mm in most cases (10/16) and 1–5 mm in some cases (6/16), for which the risk of recurrence was basically minimal and which would not have any impact on survival. Although MPD and extra-MPD are fundamentally different biological entities, in cases of extra-MPD, the level of invasion into the underlying dermis was significantly associated with reduced survival [8]. This can be applied to MPD because deeper invasion of MPD without underlying invasive BC was associated with LN metastases [4, 5] and distant recurrence [6]. In the present case, due to a deeper (2.5 mm) and larger invasive focus in the dermis (1.5 cm) than that of the cases reported by Lee et al. [2], there might be a significant risk of recurrence despite the absence of underlying invasive BC; therefore, in the present case, hormonal therapy with tamoxifen was administered.
CONFLICT OF INTEREST STATEMENT
None declared.



