-
PDF
- Split View
-
Views
-
Cite
Cite
Jeffrey D. Howard, Peter G. Deveaux, Syndrome of inappropriate antidiuretic hormone associated with rectal small cell neuroendocrine carcinoma: a case report, Journal of Surgical Case Reports, Volume 2017, Issue 7, July 2017, rjx136, https://doi.org/10.1093/jscr/rjx136
Close - Share Icon Share
Abstract
Neuroendocrine tumors can arise from any portion of the gastrointestinal tract including the colon and rectum. In the scope of all colon and rectal malignancies, they are a rare cause of colorectal carcinoma. Relating to their pluripotent neuroendocrine cellular origins these carcinomas can produce a variety of biologically active peptides with several resultant paraneoplastic syndromes. One of these paraneoplastic syndromes is the syndrome of inappropriate antidiuretic hormone (SIADH). In the SIADH, supraphysiologic levels of vasopressin (antidiuretic hormone, AVP) precipitates exorbitant free water retention and resultant electrolyte abnormalities, most notably hyponatremia. Herein we report a rare case of paraneoplastic SIADH from rectal small cell neuroendocrine carcinoma. To our knowledge, SIADH from rectal small cell neuroendocrine carcinoma has been reported only three times.
INTRODUCTION
Neuroendocrine tumors (NETs) arise from amine precursor uptake and decarboxylation cells, which are located throughout the gastrointestinal tract. Colon and rectal NETs are a rare occurrence and account for <1% of all colon and rectal malignancies [1]. Patients with colon and rectal NETs are typically asymptomatic or present with non-specific complaints. As such, the diagnosis is usually made via screening tests or evaluation for an unrelated reason.
Secondary to their neuroendocrine cellular origin, these tumors may produce a variety of biologically active peptides with a plethora of potential resulting paraneoplastic syndromes. Amongst these is included the syndrome of inappropriate antidiuretic hormone (SIADH). In the SIADH, abnormally elevated levels of antidiuretic hormone lead to excessive free water retention and significant electrolyte abnormalities, particularly hyponatremia. The diagnosis of SIADH is one of exclusion and is reliant on a series of findings as described by Bartter and Schwartz [2].
CASE REPORT
A 67-year-old Caucasian gentleman presented to his primary care physician with a chief complaint of hematochezia. A mass 1–2 cm above the anal verge was noted on digital rectal examination. Further historical evaluation detailed a history of progressive constipation, thin bowel movements, and an unintentional 15-pound weight loss over a 2-month period. At 50 years of age, he underwent a screening colonoscopy that was without mass or polyp. He had not undergone repeat colorectal screening since. His past medical history included seasonal allergies, hypercholesterolemia, and prostate cancer treated 17 years prior. There was no family history of known colorectal malignancy.
He was referred to a gastroenterologist who performed a diagnostic colonoscopy. A friable, exophytic mass was encountered 1 cm proximal to the anal verge. The pathology specimen stained positively with synaptophysin, chromogranin and TTF-1, which is consistent with small cell neuroendocrine carcinoma (Fig. 1).
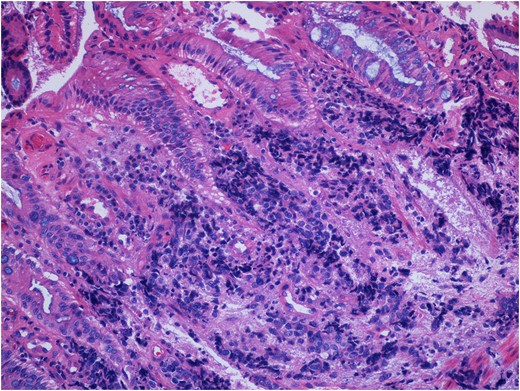
Pathologic specimen consistent with small cell neuroendocrine malignancy of the rectum. This specimen stained positively for synaptophysin, chromogranin and TTF-1 (not shown). Not seen in this image is a significant necrotic contribution consistent with high-grade pathology.
He was subsequently referred to a colon and rectal surgeon. Prior to this appointment, he was admitted to a small community hospital with abdominal discomfort and leukocytosis. Records from this facility demonstrated admission serum sodium of 122 mEq/L for which he was given two liters of intravascular normal saline. Laboratory evaluation was not repeated before his transfer to our hospital.
He was transferred to our institution the following day. At that time, he had a temperature of 36.5°C, pulse of 107 beats per minute, blood pressure of 135/62 mm/Hg, respiratory rate of 15 breaths/min, and an oxygen saturation of 94% on room air. His physical examination was remarkable for a palpable lower abdominal mass, a palpable rectal mass, and absence of peripheral edema. Serum laboratory evaluation returned the following results: hemoglobin level of 10.5 mg/dL, white blood cell count of 18 000, creatinine of 1.8 mg/dL, serum sodium of 118 mEq/L, glucose of 133 and serum osmolarity of 260 mOsm/kg. A CT scan of the abdomen and pelvis exhibited a 9.4 × 8.5 × 15.9 cm3 mass involving the posterior bladder, distal sigmoid, and proximal rectum. Urine electrolyte evaluation returned the following values: sodium of 73 mEq/L, potassium of 22.8 mEq/L and osmolarity of 432 mOsm/kg. The patient’s hyponatremia promptly resolved with fluid restriction and administration of tolvaptan, a competitive vasopressin receptor antagonist.
DISCUSSION
NETs arise from amine precursor uptake and decarboxylation cells, which are located throughout the gastrointestinal tract. Colon and rectal NETs are a rare occurrence and account for <1% of all colon and rectal malignancies. A population-based study by Bernick et al. [1] showed that ~37% of colorectal NETs occur in the rectum.
The presentation of NETs depends on their location and presence of any associated syndrome. The majority of NETs involving the colon and rectum are asymptomatic and are diagnosed during routine screening or during evaluation for unrelated reasons [3]. Potential presenting symptoms include the following: mass effect, non-specific abdominal discomfort, weight loss, bleeding, obstipation, constipation and sequelae of associated peptide production.
Due to their pluripotent neuroendocrine cellular origin, these tumors may produce a variety of biologically active polypeptides resulting in various paraneoplastic syndromes. These peptides include the following: histamine, norepinephrine, dopamine, substance P, andrenocroticotropic hormone, vasoactive intestinal peptide, growth hormone, glucagon, pancreatic polypeptide, gastrin, serotonin and vasopressin (antidiuretic hormone, AVP) [1]. The syndrome of SIADH is a known paraneoplastic syndrome of small cell neuroendocrine carcinoma. SIADH is perhaps best known and certainly best taught in relation to small cell carcinoma of the lung. In the SIADH supraphysiologic levels of vasopressin precipitates exorbitant free water retention and resultant electrolyte abnormalities, most notably hyponatremia. Symptoms of SIADH are related to the plethora of symptoms resulting from the hyponatremia.
The diagnosis of SIADH is based upon fulfillment of clinical and laboratory criteria as described by Bartter and Schwartz. Our patient fulfilled each of these criteria: (i) hyponatremia in the setting of hypo-osmolality, (ii) excessively concentrated urine, (iii) euvolemia, (iv) excessive urine sodium secretion and (v) lack of other causes of hyponatremia. The principle problem being from water retention, SIADH is treated by free water restriction and recently by the administration of competitive vasopressin receptor antagonists such as tolvaptan.
CONCLUSION
We present this case to highlight a rare presentation of SIADH from an also rare rectal small cell neuroendocrine carcinoma. To our knowledge, SIADH from rectal small cell neuroendocrine carcinoma has been reported only three times [4–6]. Our patient’s SIADH was easily corrected with a combination of free water restriction and administration of a vasopressin receptor antagonist.
CONFLICT OF INTEREST STATEMENT
None declared.



