-
PDF
- Split View
-
Views
-
Cite
Cite
Saqib Saeed, Sara Alothman, Amrita Persaud, Sanjiv Gray, Leaque Ahmed, Successful laparoscopic repair of gastro-gastric fistula following Roux-en-Y gastric bypass at Harlem Community Hospital, Journal of Surgical Case Reports, Volume 2017, Issue 7, July 2017, rjx134, https://doi.org/10.1093/jscr/rjx134
Close - Share Icon Share
Abstract
Gastro-gastric fistula is a communication between the gastric remnant and gastric pouch. It is a rare complication of Roux-en-Y gastric bypass. It is caused by anastomotic leak, marginal ulcers, distal obstruction or erosion from foreign body. In this case report, we are presenting a successful laparoscopic repair of gastro-gastric fistula in a patient who presented with weight gain after initial loss.
INTRODUCTION
Currently, bariatric surgery offers the most sustained and significant weight loss in the morbidly obese patients [1]. Indications for bariatric surgery are severe obesity with a body mass index (BMI) > 40 or > 35 in the presence of weight-related comorbid disease [2].
Laparoscopic Roux-en-Y gastric bypass (RYGB) is the most commonly performed bariatric operation in the United States [3]. Because of the advantages of minimally invasive surgery it is now the preferred surgical approach [4]. However, the procedure is not without complications.
Major complications include leaks, anastomotic strictures, bowel obstruction, gastro-gastric and gastro-cutaneous fistulas [5].
Gastro-gastric fistula, a communication between the gastric pouch and gastric remnant, is a rare complication of RYGB that can lead to weight regain, reflux and marginal ulceration.
Possible etiologies include technical complication due to incomplete division of the stomach during the creation of the pouch, or after a staple-line failure, developing a leak with resulting abscess, which then drains internally into the distal stomach forming the fistula [6]. We present a case of gastro-gastric fistula following gastric bypass at an outside facility which was successfully managed laparoscopically at our institution.
CASE REPORT
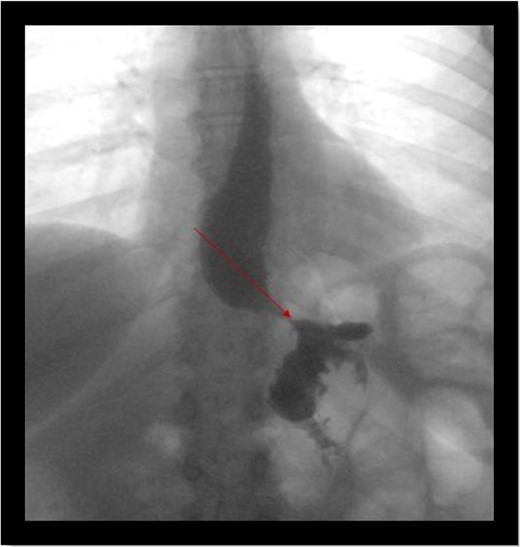
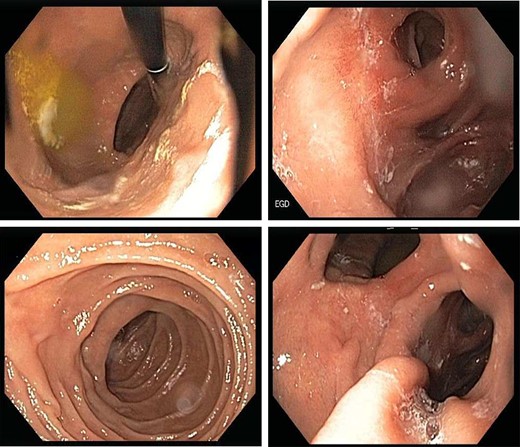
A 49-year-old female who was status post laparoscopic gastric bypass at an outside facility in 2010 presented to our bariatric clinic for evaluation. She lost 99 lb in 2 years after her gastric bypass but regained 43 lb in a couple of months prior to presentation. At the time of evaluation, patient’s BMI was 32. Upper gastrointestinal swallow study was negative for any acute abnormality (Fig. 1). Endoscopic gastroduodenoscopy (EGD) was performed which showed a communication between the gastric pouch and remnant stomach (Fig. 2). Gastric pouch was found to be 5 cm from the GE junction.
Patient was scheduled for laparoscopic repair of fistula. Intra-operatively gastro-gastric fistula was confirmed by insufflating air through gastric pouch while alimentary limb was clamped. After confirmation, remnant stomach was mobilized and transected proximally along with gastro-gastric fistula. Gastric pouch and alimentary limb were protected.
Patient tolerated the procedure well and was successfully extubated at the end of the procedure. She was discharged on post-operative Day 2. On follow-up, her BMI decreased from 32 to 28 in 3 months and she had no complaints related to the gastrointestinal tract.
DISCUSSION
The incidence of gastro-gastric fistula decreased as the REYGB technique was modified [7]. Currently, the incidence of gastro-gastric fistula ranges from 0 to 6% of RYGBs [8–10].
It is a technical complication that can be caused by incomplete division of the stomach during the creation of the pouch especially at the angle of His as the stomach can hide in the intra-abdominal fat in that area. To avoid this, it is crucial to visualize the whole stomach.
It can also occur after a staple-line failure, with resulting leak or abscess that can internally drain into the gastric remnant.
Cucchi et al. observed six patients with gastro-gastric fistulas. All patients had fever, tachycardia and abdominal pain. Less frequent symptoms were nausea, vomiting, fatigue and diarrhea, shoulder pain, tachypnea and anorexia [8]. Gastro-gastric fistula can be diagnosed early in the post-operative period when the patients fail to lose weight or late when weight regain occur as patients lose the discomfort associated with gastric pouch distention.
The diagnosis can be made using upper gastrointestinal contrast series or CT with contrast flowing into the gastric remnant. While definitive study is upper endoscopy. Once diagnosed, gastro-gastric fistula is treated surgically, by laparoscopic or open surgery.
When safe, laparoscopic surgery is preferred over open surgery for treating gastro-gastric fistula resulting in resolution of symptoms and improved weight loss with acceptable morbidity compared with patients who underwent open surgery [11].
Laparoscopic surgery is easily performed when the gastro-gastric fistula is diagnosed early in the post-operative period [12]. But when diagnosed late, the surgical approach is more difficult. When a patient present with weight regain after RYGB it is important to consider gastro-gastric fistula as a possible cause of weight regain.
ACKNOWLEDGMENT
We thank the bariatric team at our hospital.
CONFLICT OF INTEREST STATEMENT
None declared.



