-
PDF
- Split View
-
Views
-
Cite
Cite
Alessandro Tamburrini, Adnan Raza, Aiman Alzetani, Giant spontaneous herniation of the post-pneumonectomy cavity, Journal of Surgical Case Reports, Volume 2017, Issue 7, July 2017, rjx132, https://doi.org/10.1093/jscr/rjx132
Close - Share Icon Share
Abstract
Following a pneumonectomy, excessive mediastinal shift can cause rare complications involving the post-pneumonectomy cavity, which can become the seat of herniation of the residual lung and of the heart. We herein report an even more rare event, entailing an impressive herniation of the actual entire post-pneumonectomy cavity through an intercostal space, which developed spontaneously nearly 3 years after surgery. Surgical excision of the hernia sac and repair of the defect with polypropylene mesh provided adequate treatment and good cosmetic results. Postoperative recovery was uneventful and no signs of recurrence have been observed.
INTRODUCTION
Following a pneumonectomy, extreme mediastinal shift can occasionally result in overdistension and complete herniation of the remaining lung into the residual pleural cavity [1]. Cardiac herniation is another rare complication, more often described after intrapericardial pneumonectomy [2]. We herein report a very rare occurrence: a giant and symptomatic hernia of the entire post-pneumonectomy cavity through an intercostal space, developed spontaneously nearly 3 years after surgery.
CASE REPORT
An 83-year-old man, who had undergone a left pneumonectomy for primary lung cancer 33 months earlier, presented in our clinic complaining of several weeks history of significant weight loss, dyspnea and a progressively increasing and painful swelling of his left chest. Physical examination revealed an impressively large, soft and balottable mass located at the level of the previous left thoracotomy (Fig. 1). Chest computed tomography (CT)-scan showed extensive herniation of the post-pneumonectomy cavity through the rib spaces, contained by the pleura (Fig. 2A–D). The patient denied recent history of chest trauma or episodes of violent cough, and all laboratory tests, including inflammatory markers, were unremarkable. Given the size of the herniation and the patient’s progressively worsening symptoms, surgical treatment for this unusual condition was deemed necessary. Surgery was carried out via a standard postero-lateral thoracotomy at the level of the old incision. The massive pleural hernia sac was immediately evident (Fig. 3A) and, once opened, ~1700 ml pleural fluid of gelatinous consistence was aspirated. The herniation site was identified in the previously opened intercostal space, in an antero-lateral position (Fig. 3B). The large sac (21 × 18 cm2) was excised and removed (Fig. 3C), while the defect was repaired with a polypropylene mesh, fixed by interrupted sutures and covered with the edge of the adjacent serratus anterior muscle (Fig. 3D). Histology results of the pleural hernia specimen showed inflammatory changes and granulation tissue. Postoperative recovery was uneventful and patient was discharged with minimal pain after 72 h, with an elasticated vest to be worn for 6 weeks. At 6-month follow-up, patient is well and there is no evidence of recurrence.
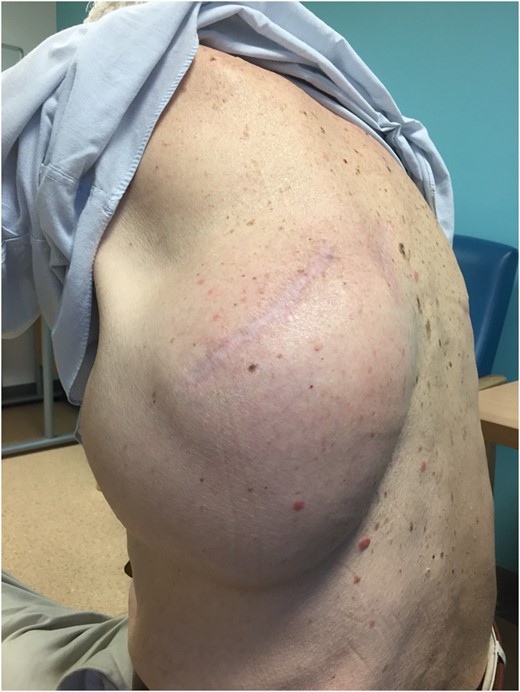
Clinical presentation of the giant post-pneumonectomy cavity herniation.
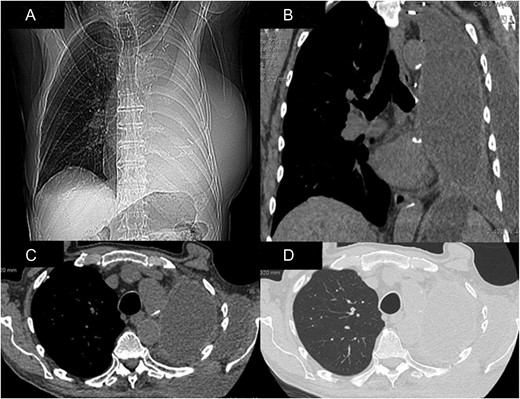
CT-scan demonstrating the impressive hernia in coronal views (A and B) and axial views (C and D).
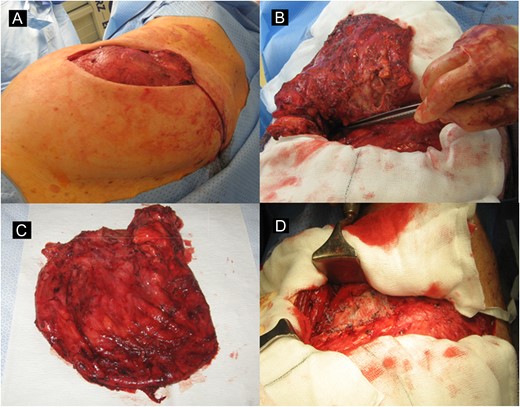
Pleural hernia sac appearance after the thoracotomy incision (A), intercostal herniation site pointed by surgeon’s forceps (B), excised hernia sac (C) and appearance of the defect after repair with polypropylene mesh (D).
DISCUSSION
Pneumonectomy for malignant disease is still considered a high-risk operation, associated with significant postoperative morbidity and mortality. Commonly described complications include adult respiratory distress syndrome, sepsis, pneumonia, arrhythmias, myocardial infarct, empyema and bronchopleural fistula [3]. Following removal of the lung, the natural evolution of the pleural cavity entails gradual accumulation of fluid and progressive shrinkage of the residual space. This leads to elevation of the ipsi-lateral hemidiaphragm, hyperinflation of the controlateral lung and shifting of the mediastinum, ultimately resulting in the obliteration of the post-pneumonectomy space. Rarely, complications of the post-pneumonectomy cavity driven by excessive mediastinal shift can occur. Herniation of the hyperinflated lung into the residual cavity and extreme rotational displacement of the mediastinum can occasionally cause the ‘Postpneumonectomy Syndrome’, a symptomatic airway compression, requiring surgical treatment [1]. Even rarest events concerning post-pneumonectomy cavity have been reported, such as ‘disappearence’ of the space [4] and occurrence of cancer [5]. Our case distinctly differs from any previously described rare complications, as we observed the herniation of the actual entire post-pneumonectomy cavity through an intercostal space. Quite surprisingly, this occurrence was not even associated with marked overdistension of the right lung, neither with any significant mediastinal rotation. A single similar case has been described by Benhamed et al. [6], who reported on a small traumatic herniation of the postpneumonectomy cavity 47 years after surgery. However, there are prominent differences between the two cases. In first instance, the size of the hernia in our patient was remarkably large, symptomatic in terms of pain and shortness of breath, as well as being the most probable cause of weight loss. These features were consistent with another relatively rare condition, yet more commonly described: chest wall hernias [7]. Furthermore, there was apparently no triggering event like a chest trauma or a vigorous cough, which are known to cause intercostal lung hernia [8]. We could therefore assert that in our case, the herniation occurred spontaneously. In conclusion, we have described a giant spontaneous and symptomatic hernia of the post-pneumonectomy cavity through an intercostal space, which appears to be more of a unique rather than a rare occurrence. Excision of the hernia sac and repair with a polypropylene mesh in line with the general surgical principles for hernia management resulted in satisfactory treatment. One should thus be aware that post-pneumonectomy cavity herniation through an intercostal space may develop spontaneously, and be even of very large proportions. Surgical repair is feasible and good results can be achieved in terms of both treatment and cosmetic.
CONFLICT OF INTEREST STATEMENT
None declared.



