-
PDF
- Split View
-
Views
-
Cite
Cite
Jeffrey J. Yu, Michael Morell, John G. Lee, David K. Imagawa, A case report on a rare anatomic variant of cystic duct insertion, Journal of Surgical Case Reports, Volume 2017, Issue 7, July 2017, rjx131, https://doi.org/10.1093/jscr/rjx131
Close - Share Icon Share
Abstract
We report a case a 70-year-old female presenting with abdominal pain who has a cystic duct coursing medial to the common bile duct before anastomosing just proximal to the ampulla. Low medial insertion of the cystic duct is a rare anatomic variant that is easily misidentified on imaging studies and may complicate surgical and percutaneous intervention. It can be identified by pre-operative imaging modalities such as magnetic resonance cholangiopancreatography.
INTRODUCTION
Variations in the course and insertion of the cystic duct are common and can complicate surgical procedures. In particular, low medial insertion of the cystic duct into the common hepatic duct can be misidentified on imaging and may increase the risk of iatrogenic injury. We present 70-year-old female with an exceedingly rare anatomical variant identified on magnetic resonance cholangiopancreatography (MRCP) who underwent open cholecystectomy.
CASE REPORT
A 70-year-old Caucasian female with a history of peripheral vascular disease and perforated peptic ulcer disease presented to the emergency room with chronic left upper quadrant abdominal pain of 7–8 months duration which had acutely worsened over the previous 4–5 days. She described the pain as ‘stabbing’ pain that radiated to her back. She reported that the pain was exacerbated by oral intake. Although the patient was having regular bowel movements without gross blood, she was noted to have microscopic blood in her stool and was sent for evaluation in the ER. Computerized tomography (CT) with contrast demonstrated evidence of fatty liver, diffuse gallbladder wall thickening, an 8 mm common bile duct, diverticulosis and a normal appendix. Lipase level was found to be within normal limits and there was no leukocytosis. The patient was subsequently transferred to our hospital for further workup.
Previous workup for the patient’s abdominal pain included a CT which demonstrated medial insertion of the cystic duct and a positive hepatobiliary iminodiacetic acid scan suspicious for cystic duct obstruction. Esophagogastroduodenoscopy (EGD) with biopsy demonstrated mild inflammation of the gastric antrum but showed no evidence of dysplasia, malignancy or Helicobacter pylori infection.
MRCP performed during the patient’s hospital stay confirmed the patient’s aberrant ductal anatomy, showing a cystic duct coursing parallel and medial to the common bile duct before anastomosing just proximal to the ampulla. CT angiogram did not show evidence of bowel ischemia.
Although the location in the left upper quadrant was not typical of gallbladder pain, cholecystectomy was offered to the patient given the evidence of gallbladder wall thickening. Additionally, workup for alternative etiologies of the abdominal pain, including mesenteric ischemia, had been negative. Patient elected to undergo open cholecystectomy with awareness that her aberrant anatomy put her at increased risk of common bile duct injury as well as the fact that her pain may not be improved by the surgery.
Patient successfully underwent EGD with stent placement in preparation for surgery. During surgery, laparoscopic examination revealed adhesions between the colon, colonic mesentery, the underside of the liver and the gallbladder due to prior surgery for her perforated duodenal ulcer. Following extensive lysis of adhesions, a top-down dissection of the gallbladder was performed. The cystic duct was once again seen coursing posterior to the common bile duct within the porta hepatis. Intraoperative cholangiogram confirmed low insertion of the cystic duct and dilation of the common bile duct. The surgery was performed without complications.
The patient’s post-operative course was without complication, with the patient tolerating oral intake and with pain managed on oral medications. However, the patient continued to complain of left-sided abdominal pain despite surgery.
DISCUSSION
The cystic duct normally joins the common hepatic duct approximately halfway between the porta hepatis and the ampulla of Vater from a right lateral position. Variations in the course and insertion point of the cystic duct are common and are often of no clinical significance. However, the aberrant cystic duct can be involved in a variety of primary and secondary disease processes and may be the source of complications during surgical or percutaneous intervention. The risk of iatrogenic injury is especially high in cases where the anatomy is misidentified prior to surgery.
The entry point of the cystic duct relative to the common hepatic duct is highly variable. The cystic duct courses parallel to the common hepatic duct in 10.6% of patients. There is insertion from the medial aspect in 18.4% of patients and distal insertion in 10%. In a study of 198 patients who underwent MRCP, 4% were found to have a low medial insertion [1]. However, low insertion in this study was defined as the cystic duct joining the common hepatic duct at its lower third, whereas in this case, the cystic duct joined the common hepatic duct just proximal to the ampulla. The particular variation of a medial insertion at the level of the ampulla as seen in this case is an exceedingly rare finding. Other variations in cystic duct anatomy include anterior or posterior spiral insertion, proximal insertion and more rarely joining the left or right hepatic duct high in the porta hepatis or directly into the duodenum [2, 3].
Low, medial insertions of the cystic duct as seen in this patient are particularly susceptible to misdiagnosis on imaging given the tendency of the cystic duct to overlie the common bile duct. This may cause inadvertent ERCP stent placement into the cystic duct rather than the common bile duct, as well as a host of other complications during stone retrieval. Furthermore, cystic duct remnants associated with low medial insertion tend to be longer than normal due to encasement in a common sheath with the common hepatic duct [4].
While ultrasound and CT are able to detect dilated cystic ducts, normal cystic ducts with diameters in the range of 1–5 mm are often not detected with these modalities. MRCP is an accurate imaging modality in detecting aberrant ductal anatomy, demonstrating a cystic duct in 74% of patients [5]. Direct cholangiography, including ERCP and intraoperative cholangiography, is invasive but readily identifies anatomical variations. In this case, MRCP correctly identified the course and insertion of the cystic duct relative to the common hepatic duct (Fig. 1).
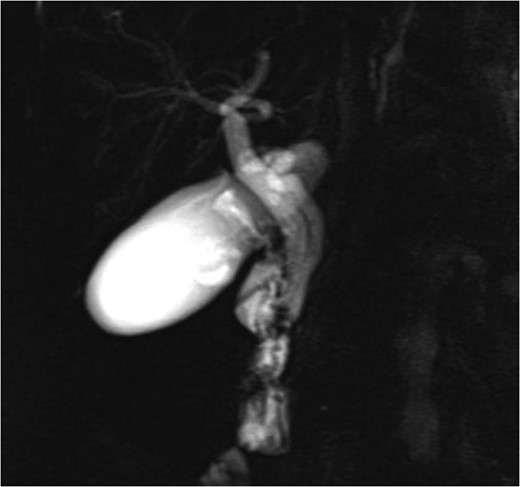
MRCP image showing long parallel course of the cystic duct inserting medially just proximal to the ampulla of Vater.
In conclusion, cystic duct anatomy variants may complicate cholecystectomy and can be identified by pre-operative imaging modalities such as MRCP. It is particularly important to identify low medial insertion of the cystic duct, as seen in this case, prior to intervention in order to prevent iatrogenic injury.
CONFLICT OF INTEREST STATEMENT
None declared.



