-
PDF
- Split View
-
Views
-
Cite
Cite
S. M. Mohar, Saqib Saeed, Alexius Ramcharan, Hector Depaz, Small bowel obstruction due to mesenteric abscess caused by Mycobacterium avium complex in an HIV patient: a case report and literature review, Journal of Surgical Case Reports, Volume 2017, Issue 7, July 2017, rjx129, https://doi.org/10.1093/jscr/rjx129
Close - Share Icon Share
Abstract
Small bowel obstruction in HIV patients is reportedly caused by inflammatory pseudotumor, Kaposi’s sarcoma, cryptococcal lymphadenopathy and intestinal tuberculosis. The incidence of Mycobacterium avium complex (MAC) infection in HIV patients is 3% for CD4 cell count of 100–199 /mm3. MAC causing small bowel obstruction is rarely reported in the literature. We report a rare case of MAC causing mesenteric abscess with small bowel obstruction in a HIV patient with a CD4 cell count of 144 /mm3. Patient was a 35-year-old HIV-positive male on highly active antiretroviral therapy who presented with partial small bowel obstruction secondary to mesenteric abscess. He underwent operative intervention for drainage with cultures growing MAC.
INTRODUCTION
Mycobacterium avium complex (MAC) is one of the most serious opportunistic infection in HIV patients. The incidence of MAC infection in HIV patients is 3% for CD4 cell Count ranging from 100 to 199/mm3 [1]. It can cause variety of complications. Small bowel obstruction in HIV patients is reportedly caused by inflammatory pseudotumor [2], Kaposi's sarcoma [3], cryptococcal lymphadenopathy [4] and intestinal tuberculosis [5].
We are reporting a rare case of mesenteric abscess caused by MAC in HIV patient with a CD4 cell count of 144 /mm3 resulting in small bowel obstruction.
CASE REPORT
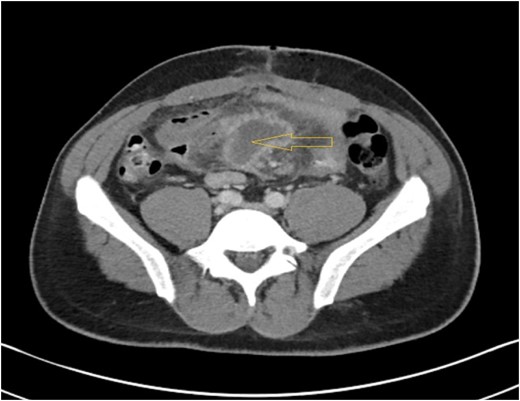
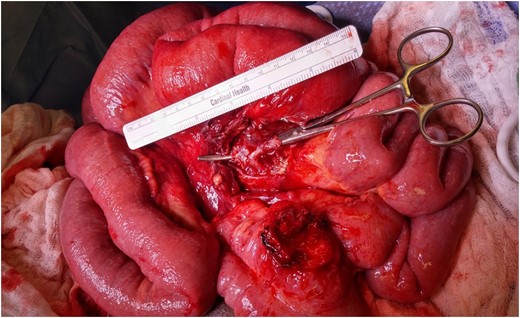
A 35-year-old HIV positive male on highly active antiretroviral therapy (HAART) presented to the Emergency room with progressive colicky abdominal pain for 7 days. Pain had gotten diffuse over this time with increased abdominal distension, nausea and bilious vomiting. Patient had no previous abdominal surgery or radiation. Laboratory results revealed a white blood cell count of 5.2 103 /μL, neutrophil 49.1%, hemoglobin 12.3 g/dL, hematocrit 39.4, platelet count of 247 103 /μL. Serum lactate, amylase and lipase levels were normal. X-ray of the abdomen demonstrated dilated small bowel loops within the mid-abdomen measuring approximately 4.5 cm in maximal transverse diameter, highly suggestive of partial small bowel obstruction. A double contrast CT scan of abdomen and pelvis (Fig. 1) showed partial small bowel obstruction with thickened loop of ileum and interloop abscess measuring 3.7 × 3.2 × 5.3 cm3 with diffuse mesenteric lymphadenopathy. Initial management consisted of NG tube suction, nil peros and intravenous (IV) fluid resuscitation. He received ciprofloxacin, metronidazole, vancomycin, sulfamethoxazole/trimethoprim (for pneumocystis jerovechi pneumonia prophylaxis), emtricitabine/tenofovir disoproxyl fumerate; darunavir; ritonavir and ethambutol. By hospital day four his condition did not improve with conservative management. At this time, decision was made to explore the abdomen. During the procedure, adhesiolysis and drainage of an 8 cm mid-ileal mesenteric abscess was performed (Fig. 2). Adhesive bands between the wall of the abscess and ileum compressing the underlying ileum were divided. The appendix appeared to be normal. Abscess materials were sent for microbiological cultures which grew MAC. A separate mesenteric lymph node biopsy was performed which showed reactive lymphadenopathy. Patient was discharged on postoperative Day 3 with oral antibiotics but he got readmitted the next day with complaints of abdominal pain, nausea and vomiting. A repeat CT scan of abdomen was performed which showed postoperative ileus, for which he was managed conservatively. He was discharged 2 days later with improvement of symptoms of nausea and vomiting. At 6 months follow up, he remained asymptomatic on HAART therapy with no evidence of gastrointestinal disturbance.
DISCUSSION
MAC consists of several related species of Mycobacterium that are normally found in the environment. MAC rarely causes disease in humans with healthy immune system. In patients with AIDS, however, it is one of the most common and serious opportunistic infection. In HIV-infected individuals, disseminated MAC has occurred almost exclusively in patients with a CD4 count <50 cells/μL [6]. Colonization of the respiratory and gastrointestinal tract by MAC can remain asymptomatic but indicates increase risk for developing disseminated MAC infection [1]. Lungs are the most common organs affected but localized disease such as lymphadenopathy or lymphadenitis can also present. Intra-abdominal complications by MAC are very rare. MAC is diagnosed by identifying the organism by cultures or by biopsy. The Best way to treat disseminated MAC is to prevent it in first place. Combination antiretroviral therapy (ART) has been associated with reductions in AIDS-related mortality, days of hospitalization, and the incidence of new opportunistic infections [7]. There is convincing evidence that optimal treatment of disseminated MAC infection improves survival and quality of life [8]. The treatment regimen for disseminated MAC should include at least two drugs to prevent emergence of resistance. The newer macrolide antibiotics, clarithromycin and azithromycin are proved to be the most efficacious drugs for the treatment of MAC [9]. The optimal treatment regimen should include one of these agents along with ethambutol and/or rifabutin [10]. Efficacy results of randomized controlled trials indicate that clarithromycin, azithromycin, or rifabutin prophylaxis should be administered to prevent MAC disease in all HIV-infected patients with a CD4 count <50 cells/μL [11]. Two randomized controlled studies have compared azithromycin with placebo in patients with CD4 counts >100 cells/μL on ART and no prior history of disseminated MAC [12]. Our case is a rare case of MAC causing a mesenteric abscess with small bowel obstruction in a HIV patient with a CD4 cell count of 144/mm3. In our case, the question remains as to how long should secondary prophylaxis be continued and at what level (CD4 count) should it be discontinued. Another factor that needs to investigated is whether the MAC infection is changing its virulence. In patients with HIV infection presenting with bowel obstruction, opportunistic pathogens including MAC should be considered. Partial small bowel obstruction in such patients maintained on HAART should raise the suspicion of MAC mesenteric abscess. There should be a low threshold for drainage, especially in a patient with no previous abdominal operation. Our patient underwent a laparotomy for drainage of the abscess and lysis of adhesions. He received HAART along with sulfamethoxazole/trimethoprime for pneumocystis jerovechi pneumonia prophylaxis and ethambutol/clarithromycin for Mycobacterium avium intracellular complex treatment. Outcomes were favorable.



