-
PDF
- Split View
-
Views
-
Cite
Cite
Katherine A. Smith, Jeffrey P. Fleming, Robert D. Bennett, Andrew A. Taitano, A case of fatal internal jugular vein perforation during nasogastric tube insertion, Journal of Surgical Case Reports, Volume 2017, Issue 7, July 2017, rjx128, https://doi.org/10.1093/jscr/rjx128
Close - Share Icon Share
Abstract
Nasogastric tube (NGT) insertion is a routine procedure in the management of surgical patients. We report the second case of internal jugular vein perforation during NGT insertion. A 79-year-old man presented with diffuse abdominal pain secondary to a perforated viscus. Abdominal CT revealed pneumoperitoneum, necessitating emergent exploratory laparotomy. On post-operative Day 7, the patient developed mild abdominal distension and subjective nausea for which NGT placement was ordered for decompression. Tube placement was confirmed by insufflation of air without aspiration of gastric contents. Output from the NGT upon placement revealed frank blood. The patient then developed respiratory distress requiring intubation, followed by a fatal arrhythmia. Post-mortem exam revealed the trajectory of the NGT through the pharyngeal wall into the right internal jugular vein. This case illustrates the importance of systematic evaluation of all procedures, as the outcome resulted from failure to recognize the initial error in tube placement.
INTRODUCTION
Nasogastric tube (NGT) insertion is a routine component of peri-operative management of the surgical patient. This is generally a low-risk procedure, but severe consequences have been documented. We present a case of a fatal internal jugular vein perforation with NGT insertion.
CASE REPORT
A 79-year-old man with a history of hypertension, congestive heart failure, COPD, gastroesophageal reflux disease, alcohol abuse, major depression and no surgical history, presented to the emergency department with acute onset diffuse abdominal pain and distension. The patient had no nausea or vomiting prior to presentation and reported no bowel movements for four days. Physical exam revealed abdominal distension, tenderness to palpation over the right upper and lower quadrants, a reducible umbilical hernia, and an absence of peritoneal signs.
Abdominal CT showed pneumomediastinum and pneumoperitoneum secondary to perforated hollow viscus necessitating emergent exploratory laparotomy (Figs 1 and 2). Lysis of adhesions, right hemicolectomy with primary ileocolic anastomosis, and umbilical hernia repair were performed. NGT placement after induction of general anesthesia was noted to be difficult secondary to resistance met with advancement of the catheter. Postoperatively, the patient was transferred to the surgical intensive care unit (SICU) in stable condition.
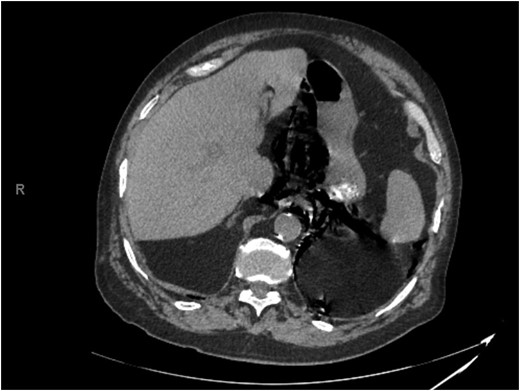
Representative slice from abdominal computed tomography imaging on admission.
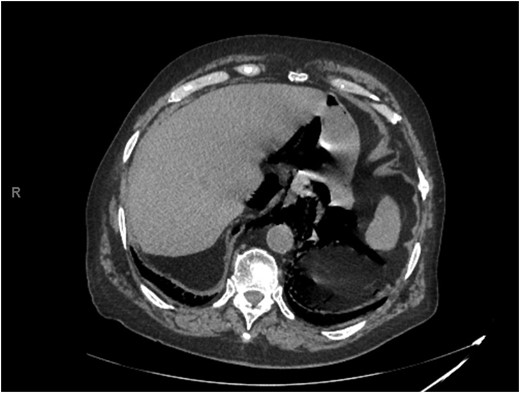
Representative slice from abdominal computed tomography imaging on admission.
The patient was transferred from the SICU to the surgical floor on post-operative day (POD) 4. The patient remained afebrile without leukocytosis. His clinical status steadily improved. Bowel function returned on POD 6. During morning rounds on POD 7, the patient felt significantly improved and was tolerating oral food intake. However, the patient developed increasing abdominal distension and tympany throughout the day. Abdominal radiographs demonstrated a dilated stomach for which NGT placement was ordered. An 18 Fr NGT was placed by nursing staff. Placement was checked by insufflation of air and auscultation over the epigastrium. Initiation of low continuous wall suction yielded 300–400 ml of dark blood. The NGT was secured in place at 50 cm at the nare when the surgeon arrived. The patient was alert and oriented at the time of exam. He denied pain or nausea. He was hypertensive with systolic blood pressures in the 160 s. The patient's history of alcohol abuse prompted concern regarding an upper gastrointestinal bleed from undiagnosed esophageal varices or bleeding peptic ulcer.
The patient subsequently became tachycardic and tachypneic. Increased work of breathing was noted with an oxygen saturation of 63%. The patient was placed on a non-rebreather mask, and his oxygen saturation subsequently increased to 99%. Shortly after the non-rebreather was placed, the patient became somnolent, responsive only to sternal rub. The patient was intubated for airway protection and plans made for transport to the SICU. Portable semi-upright chest x-ray demonstrated an endotracheal tube in proper position, no pneumothorax, and possible left pleural effusion. The tip of the NGT was not initially visualized (Fig. 3).
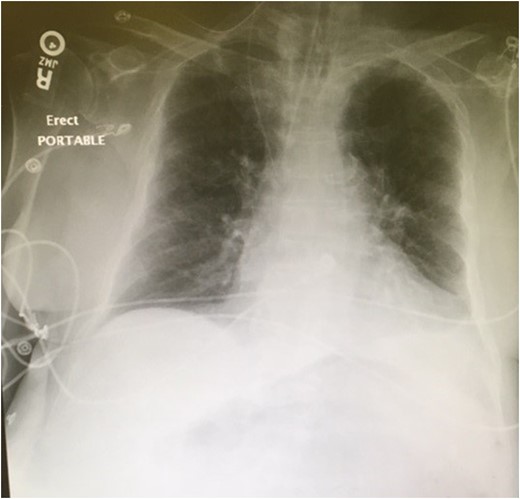
Portable semi-upright chest x-ray demonstrating an endotracheal tube in proper position, no pneumothorax, and possible left pleural effusion. No evidence of widened mediastinum or free air under the diaphragm. The nasogastric tube is visible coursing through the right internal jugular vein to the superior vena cava. The tip of the nasogastric tube is not visible.
The patient was managed empirically for a presumed upper gastrointestinal bleed with intravenous fluids and proton-pump inhibitors. Fluid resuscitation was initiated with a one liter bolus of normal saline. Type and cross was ordered for two units of packed red blood cells. A new 18 Fr NGT was placed to 60 cm in one attempt without difficulty. The new NGT continued to return gross blood. After ~2 L of blood were suctioned through the NGT, the patient developed an acute bradyarrhythmia, followed by pulseless electrical activity. ACLS protocol was initiated. The patient developed ventricular fibrillation unresponsive to electrical defibrillation, followed by asystole. Cardiopulmonary resuscitation was performed for 20 min before the patient was pronounced dead.
Postmortem evaluation demonstrated NGT placement at 65 cm at the nasal orifice. The tube crossed the midline and perforated the right lateral pharyngeal wall. The tube continued into the right internal jugular vein and terminated in the superior vena cava immediately superior to the cavo-atrial junction.
DISCUSSION
NGTs can aid in gastrointestinal decompression for patients with ileus or bowel obstruction. The tube is conventionally inserted into the nare of an alert patient and advanced to the posterior hypopharynx. The patient is then asked to swallow, and the tube is advanced through the esophagus to the stomach. If resistance is met, an attempt should be made through the contralateral nare. Once the tube is placed, position can be confirmed radiographically or clinically. Clinical confirmation of NGT placement is typically performed first by aspiration; if gastric contents are retrieved, then the tube is tested by flushing 20 ml of saline, followed by immediate aspiration. If most of the fluid is returned, then appropriate placement is considered confirmed [1].
NGT placement is contraindicated in the presence of facial or basilar skull fractures due to the risk of intracranial tube insertion [1, 2]. Other reported complications include esophageal perforation into the pleural space, perforation of the tracheobronchial tree, gastric perforation and formation of a retropharyngeal hematoma [3–6]. Few cases describe perforation of vascular structures. Creation of an aortoesophageal fistula, perforation of a large intrathoracic vessel, and perforation of an aberrant right subclavian artery have been described [7–9]. To our knowledge, Duthorn et al. [10] reported the only other known case of NGT placement into the internal jugular vein. Multiple imaging modalities including plane chest radiographs were used to identify placement in this case. Rapid hemodynamic resuscitation at the time of perforation and nasopharyngeal tamponade after NGT removal prevented patient mortality. Neither insufflation with air nor water infusion through the NGT was attempted. This removed the opportunity for additional iatrogenic damage and fatal complications. Our case highlights the importance of clinical confirmation of proper NGT placement. After insertion is complete, the contents of the tube should be immediately aspirated. If gastric contents are not obtained, then the tube should not be flushed with water or air. In our case, repeated attempts to confirm proper gastric placement of the NGT with air likely resulted in an air embolus, ultimately contributing to the patient's respiratory demise. If the tube produces bloody output, radiographic imaging should be performed immediately. The events leading to this patient’s death resulted from failure to recognize the initial error in placement. Thus, our case illustrates the importance of systematic evaluation of NGT placement and other routine procedures.
ACKNOWLEDGEMENT
This material is the result of work supported with resources and the use of facilities at the C.W. Bill Young VA Medical Center.
CONFLICT OF INTEREST STATEMENT
None declared.
DISCLAIMER
The contents of this publication do not represent the views of the U.S. Department of Veterans Affairs or the United States Government.
REFERENCES
- cardiac arrhythmia
- abdominal pain
- insufflation
- intubation
- nausea
- surgical procedures, operative
- pneumoperitoneum
- pulmonary aspiration of gastric contents
- abdominal swelling
- internal jugular vein
- respiratory distress
- nasogastric tube
- nasogastric tube placement
- laparotomy, exploratory
- abdominal ct
- perforated viscous
- right internal jugular vein
- pharyngeal wall



