-
PDF
- Split View
-
Views
-
Cite
Cite
Chadwick J. Knight, Igor Wanko Mboumi, Errington C Thompson, Severe pelvic fracture with profound hypotension: a case report and treatment algorithm, Journal of Surgical Case Reports, Volume 2017, Issue 6, June 2017, rjx093, https://doi.org/10.1093/jscr/rjx093
Close - Share Icon Share
Abstract
Approximately 9% of all blunt trauma patients suffer pelvic fractures. These fractures can range from insignificant and requiring almost no therapy to massive destruction of the pelvic ring with associated with multisystem injury and life-threatening hypotension which mandates the attention of the trauma surgeon, the orthopedic surgeon, the interventional radiologists and possibly other subspecialists. We present a case of a patient who presented to the emergency room in extremis from massive bleeding from a complex pelvic fracture. The patient developed abdominal compartment syndrome. The patient was emergently taken to the operating room but we were unable to control his pelvic bleeding. We propose an algorithm which might be helpful in these critically ill patients.
INTRODUCTION
Complex pelvic fractures can be very challenging. We present a patient with a complex pelvic fracture who would have benefitted from bilateral internal iliac artery embolizations.
CASE REPORT
A 55-year-old male arrived at the ER, a large tree having fallen across his pelvis. The patient was hypotensive at the scene. He received over 1500 ml of crystalloid in route to the emergency room. Upon arrival to St. Mary’s Medical Center, the patient had a systolic pressure of 70. His heart rate was in the 130 s. The patient was awake and alert. A left subclavian central line was placed and he was transfused with two units of O-blood. The patient’s abdomen was soft and nontender. The patient had blood at his meatus. The patient’s pelvis was tender to palpation. His left leg was cold, mottled and pulseless. There was no femoral pulse on the left side. The chest x-ray was normal, however, the pelvis film revealed extreme widening and displacement of the symphysis pubis (Fig. 1). A bedsheet was wrapped around the patient’s pelvis and another two units of O-packed red blood cells were administered. Additionally, he was given four units of fresh frozen plasma. The patient was started on norepinephrine to control his persistent hypotension. His systolic blood pressure rose into the mid-90s and the patient was taken to the CT scanner. The CT scan revealed that the patient had an acute occlusion of his left iliac artery, as well as a large left iliac wing fracture with a massive associated hematoma. A right iliac wing fracture was located near the sacroiliac joint. There was pubic diastasis, as well as a left superior rami fracture with a modest associated hematoma. There was no extravasation of dye (Figs 2 and 3). The patient was taken directly to the operating room because he was developing significant abdominal distention in the face of continued hypotension. Anesthesiologists placed a second large-bore central line for fluid resuscitation. An exploratory laparotomy was performed, revealing an intraperitoneal bladder rupture. The patient was bleeding freely from his pelvic hematoma. Multiple attempts were made to pack the pelvis tightly with laparotomy pads, but efforts were unsuccessful. Because of the distorted anatomy obtaining proximal and distal control of the iliacs was extremely difficult. The patient suffered massive retroperitoneal venous bleeding, which we were unable to control. The patient exsanguinated on the operating room table; despite having received over 30 units of packed red blood cells, 30 units of fresh frozen plasma, several 10 packs of platelets, cryoprecipitate and factor VII A.


Large retroperitoneal hematoma. Arrow depicts injured left iliac artery.

DISCUSSION
Pelvic fractures were categorized by Burgess and Young in 1990 [1]. Presenting with a very wide pubic symphysis, as well as a fracture of the iliac wing posteriorly, it appeared that this patient had an APC-III type fracture. These fractures are associated with nerve damage, organ injuries and significant bleeding [2].
The question must be asked as to what steps could have been taken in order to improve this patient’s outcome. If such a patient is to be taken to the OR, then consideration of bilateral internal iliac artery ligation should be entertained in the face of massive venous bleeding [2, 3]. Existing literature does not include a large sampling of patients with pelvic fractures who have undergone this procedure.
Intraperitoneal packing was attempted, though unsuccessful in this patient. Since the patient had ruptured his retroperitoneum and was bleeding freely into the abdomen, it was hard to see how preperitoneal packing would have helped in this particular situation. Several reports in the literature have established convincing benefits gained from preperitoneal packing [4, 5]. Preperitoneal packing, combined with pelvic fixation and/or angiography, appears to be beneficial in patients with severe pelvic fractures and massive bleeding.
With a negative FAST in the ER, one could argue that the CT scans of the abdomen and pelvis were not needed. Instead of the CT scanner, the patient could be taken to interventional radiology to undergo an angiogram with possible bilateral temporary internal iliac embolization. Velmahos published a small retrospective study in Los Angeles County, seeming to validate probable benefit from this procedure without significant complications [3]. The embolization was performed on 30 patients; bleeding was controlled in 29 of these patients. The mortality rate in this study was 33%. Nine patients died of associated injuries, multiple organ dysfunction syndrome, and/or severe head injury. In this retrospective study, no significant complications were discovered due to the bilateral internal iliac artery embolizations. In total, 13 patients had exploratory laparotomies prior to their radiological interventions. Some professionals in our industry have questioned whether this procedure causes urogenital dysfunction. In a follow-up study from the same LA group, results showed that the severe pelvic fractures themselves, rather than the procedure, were responsible for the urogenital dysfunction [6]. The authors of this study used gelatin sponges to perform the bilateral internal iliac artery embolizations. These sponges cause temporary occlusion of the arterial blood flow, which may explain the low rate for complication in this group.
Recently, a large, multi-institutional study involving 11 level I trauma centers prospectively investigated the current management of patients with severe pelvic fractures [7]. With over 1300 patients in the study, 79 subjects underwent therapeutic angioembolization. Preperitoneal packing was only used in 35 patients. And 15 of these 35 patients underwent additional procedures in order to control bleeding. None of the patients in this study received bilateral internal iliac artery embolizations to control bleeding. The mortality rate of patients who presented in shock was 32%.
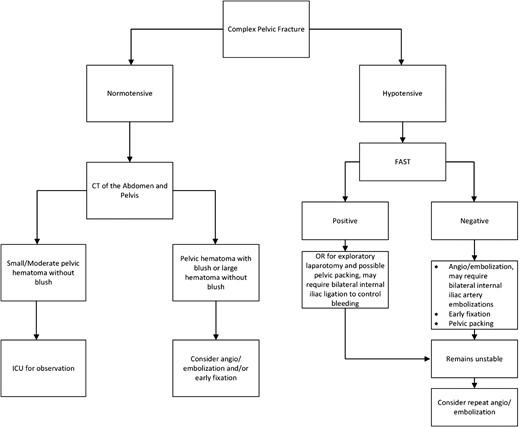
Patients who present hemodynamically unstable from complex pelvic fractures continue to be extremely challenging. Exactly which procedure should be used, and in which specific patients, is still vague and somewhat unclear from the extant literature. We propose the following algorithm based on the literature and our experience (Fig. 4).
CONFLICT OF INTEREST STATEMENT
There are no conflict of interest.
FUNDING
There were no funding or grants for this project.
REFERENCES
Author notes
Doctors Knight, Wanko and Thompson contributed equally to the planning, conduct and writing this article.



