-
PDF
- Split View
-
Views
-
Cite
Cite
Aleem K. Mirza, Audra A. Duncan, Thoracic outlet syndrome as a consequence of isolated atraumatic first rib fracture, Journal of Surgical Case Reports, Volume 2017, Issue 6, June 2017, rjx100, https://doi.org/10.1093/jscr/rjx100
Close - Share Icon Share
Abstract
Neurogenic thoracic outlet syndrome (nTOS) resulting from an isolated first rib fracture is extremely infrequent. We report a case of performance limiting nTOS in a college athlete who was initially evaluated and treated for upper extremity ligamentous injury with only transient improvement. Subsequent noninvasive studies were consistent with TOS physiology and MRA showed a large hypertrophic callus on the first rib adjacent to the brachial plexus. With continued athletic limitations and radiographic findings consistent with TOS, surgical decompression was performed resulting in resolution of symptoms. Although apparent atraumatic isolated first rib fractures are infrequently reported etiologies for TOS in athletes, they are a reasonable consideration in this population with corresponding presentations.
INTRODUCTION
Thoracic outlet syndrome (TOS) results from compression of the neurovascular bundle in the thoracic outlet and can be further specified as one of three distinct entities: neurogenic, venous, or arterial, with neurogenic being the most common [1]. Neurogenic TOS (nTOS) usually occurs as a result of extrinsic compression of the brachial plexus. This compression may occur due to congenital or acquired anomalies of the bony or soft tissue structures such as cervical ribs or hypertrophied scalene muscles [2]. Symptoms may include pain, paresthesias and weakness in the extremity and there is often a history of repetitive overhead movements or trauma [3]. However, cases of TOS resulting from fractured ribs without a history of antecedent trauma are exceedingly rare [4]. We report a case of performance limiting nTOS in a young athlete secondary to a fractured first rib without apparent preceding trauma.
CASE REPORT
An 18-year-old male college baseball pitcher and football player presented with right upper extremity pain and exertional fatigue with overhead throwing for 18 months. He also endorsed paresthesias in the right fourth and fifth fingers as well as loss of power manifested by slower pitching speeds, result in a decline in his athletic performance. Symptoms were largely absent at rest with little to no effects noticed with activity below shoulder level. He denied any shoulder pain or limitation of motion at the glenohumeral joint. There was no preceding trauma although he has a history of medial epicondyle fracture with a closed reduction 4 years prior and thoracic myofascial pain managed with ongoing physical therapy.
He was initially seen by Sports Medicine who performed an extensive work-up over a 6-month period including a negative EMG, shoulder radiographs, and MRI of the humerus and glenohumeral joint that suggested a posterior labral tear. Physical exam was unremarkable for shoulder tenderness, muscle atrophy, limitation of mobility around the glenohumeral joint or decreased strength. Noninvasive studies suggested TOS with positive costoclavicular and hyperabduction maneuvers, but due to his presentation, an injury to the glenoid labrum was suspected and they proceeded to manage his symptoms conservatively with intra-articular injections and physical therapy. Due to only transient improvements, he was referred to Vascular Surgery for evaluation.
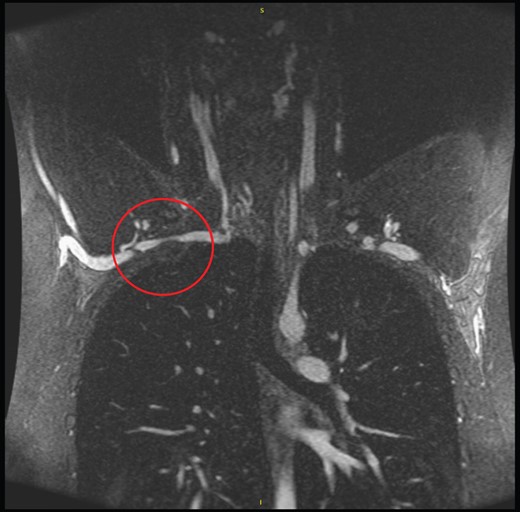
MRA of the chest showed a nonunion fracture of the right first rib with a large hypertrophic callus adjacent to the brachial plexus compressing the subclavian artery mildly (Fig. 1). No cervical rib was present. With radiographic evidence suggesting TOS, surgical decompression was offered to the patient. After discussion, the decision was made to proceed with transaxillary first rib resection.
Surgical procedure
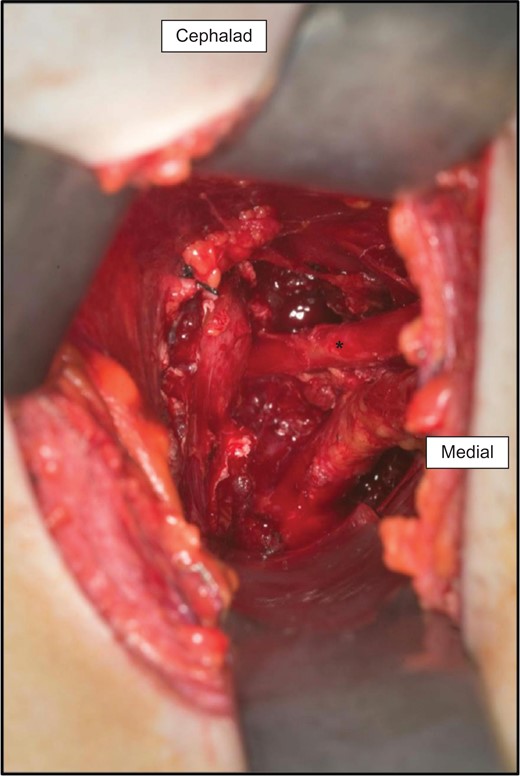
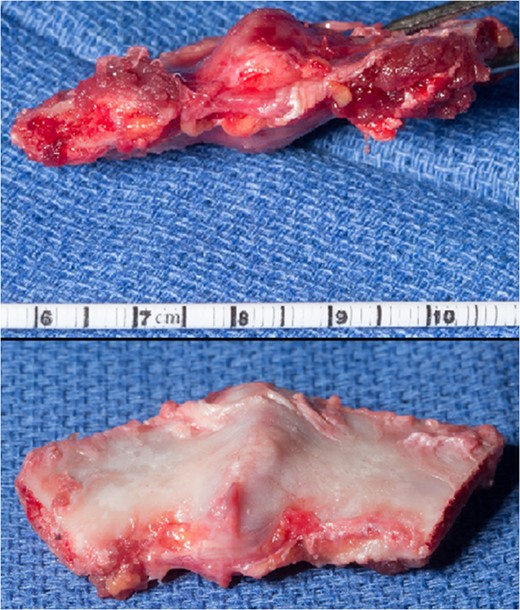
Under general anesthesia in left lateral decubitus, a transverse incision was made in the axilla with dissection carried down to the thoracic outlet. The anterior and middle scalenes were identified and resected. The large callus on the first rib was identified and located adjacent to the neurovascular bundle consistent with preoperative imaging (Fig. 2). The rib was then circumferentially isolated and resected with a rib cutter, however the posterior-most portion of the rib was inaccessible. Therefore a rongeur was used to remove remaining bone. On inspection of the specimen, a large protuberance corresponding to the callus on MR was immediately obvious (Fig. 3). The neurovascular bundle was identified and protected throughout the resection. There was obvious entrance into the chest so a chest tube was place. The patient was woken and had an intact neurological and vascular exam. Postoperative chest film showed adequate removal of the first rib.
On postoperative Day 1, his chest tube and drain were removed and he was discharged home without any issues. At his 5-month follow up visit, his paresthesias had completely resolved and he denied exertional fatigue. He had resumed pitching and endorsed marked improvement.
DISCUSSION
nTOS occurs as a result of extrinsic brachial plexus compression in the scalene triangle as in the case described. When compression occurs in the pectoralis minor space, this is referred to as neurogenic pectoralis minor syndrome (NPMS). Compression of the plexus in both spaces is described as nTOS/NPMS. Per reporting standards of the Society for Vascular Surgery, nTOS is defined by the presence of at least three of four criteria: local findings with history and physical findings of pain around the thoracic outlet, peripheral findings consistent with brachial plexus compression, exclusion of other possible diagnoses or a positive scalene injection test [5].
Patients with nTOS commonly endorse history of trauma to the neck or shoulder [1, 3]. Clavicular or rib fractures causing TOS have been described, but most frequently in the setting of motor vehicle accidents [6], and infrequently in athletes [7]. In fact, isolated traumatic rib fractures in athletes without resulting TOS are rare, further underscoring the infrequent incidence of subsequent TOS in this population [8, 9].
Prior reports describe fatigue fracture as part of the mechanism of injury, due to repetitive contraction of the scalene muscles weakening the first rib, with subsequent stress fracture from physical contact during sports activities [4]. In our case, it is plausible to suspect that an element of fatigue fracture contributed to the mechanism of injury as the patient is a competitive baseball pitcher. Although no discrete trauma to the neck or shoulder was reported, he certainly may have suffered an impact from a subsequent event compounding the insult to the first rib, as described in prior reports [4].
Initial conservative management with injection and rehab for suspect labral tear was certainly congruent with conservative therapy for nTOS [1], but unfortunately provided only transient relief with continued athletic limitation. Therefore, with an obvious source for compression radiographically confirmed, and reproducible symptoms with provocative maneuvers, we felt surgical decompression with first rib resection and scalenectomy was reasonable. As with previously reported cases [4], we elected for a transbrachial approach as this allowed abundant exposure and access to the first rib and scalenes as well as visualization and protection of the neurovascular structures (Fig. 1).
Although apparent atraumatic isolated first rib fractures are infrequently reported etiologies for TOS in athletes, they are a reasonable consideration in this population with corresponding presentations.
CONFLICT OF INTEREST STATEMENT
None declared.



