-
PDF
- Split View
-
Views
-
Cite
Cite
Hossam Abdulghafar, Ibrahim Naif Almutairi, Rouz Faisal Abu Sulami, Abdullah Khalid Aljohani, Suha Mutasim Al Haj, Symptomatic hemorrhagic mesenteric cyst: case report, Journal of Surgical Case Reports, Volume 2025, Issue 12, December 2025, rjaf999, https://doi.org/10.1093/jscr/rjaf999
Close - Share Icon Share
Abstract
Hemorrhagic mesenteric cysts are benign tumors that originate from the mesentery. They are rare, with a reported incidence of 1 in 100 000. They are often asymptomatic but can present with abdominal pain, a palpable abdominal mass, or even intestinal obstruction. Complete surgical excision is crucial to ensure optimal recovery and minimize recurrence. We present a case of a 55-year-old male patient with a history of progressive abdominal pain over a period of 10 days. Accompanied by abdominal distension, constipation, nausea, and vomiting. Physical examination revealed tachycardia, abdominal distension, and generalized tenderness. A computed tomography scan revealed a large lobulated mass with internal mixed high attenuation, suggestive of hemorrhagic content, with signs of upper gastrointestinal obstruction. The patient underwent an emergent exploratory laparotomy. Intraoperatively, a hemorrhagic mesenteric cyst was found in the mesentery of the small bowel, originating at the duodenojejunal junction. The postoperative course was uneventful.
Introduction
Mesenteric cysts are benign tumors originating from the mesentery of the small bowel in 66% of cases and the large bowel in 33% [1]. They are rare, with a reported incidence of 1 in 100 000, with a female-to-male ratio of 2:1 [2]. Hemorrhagic mesenteric cysts are often asymptomatic and discovered incidentally during routine imaging. It may present with acute or chronic abdominal pain, palpable abdominal mass, abdominal distension, nausea and vomiting, constipation, or diarrhea [2]. Other complicated presentations include intestinal obstruction, volvulus, and peritonitis [3]. Complete surgical excision, whether performed openly or laparoscopically, is crucial to ensure optimal recovery and minimize recurrence [4]. Our case report describes the case of a 55-year-old male patient who presented with acute abdominal pain and distension. Underwent an emergent exploratory laparotomy, and histopathological examination of the cyst revealed a benign hemorrhagic mesenteric cyst.
Case report
A 55-year-old male with no significant medical or surgical history, and no previous trauma to the abdomen. Presented to the emergency department complaining of progressive abdominal pain over a period of 10 days. Accompanied by abdominal distension, constipation, nausea, and vomiting. That became worse in the last 4 days before presenting to the hospital. Physical examination revealed a tachycardia with a heart rate of 120 beats/min, other vital signs were stable.
On local examination, there was abdominal distension with generalized tenderness mainly at the epigastrium region, with a hyperresonant abdomen on percussion.
Laboratory tests revealed leukocytosis with a white blood cell (WBC) count of 11.8 × 109/L, normocytic normochromic anemia with a hemoglobin level of 10.9 g/dL, mean corpuscular volume (MCV) 87 fL, mean corpuscular hemoglobin concentration (MCHC) 34 g/dL, thrombocytosis with a platelet count of 487 × 109/L, hypokalemia with a potassium level of 2.8 mEq/L, a high creatinine level of 121 umol/L, a low albumin level of 31 g/L, a high amylase level of 120 U/L, a normal lipase level.
A contrast-enhanced computed tomography (CT) scan of the abdomen revealed a large, lobulated mass measuring 7.5 cm in the anterior–posterior dimension, 15 cm in the transverse dimension, and 16 cm in the craniocaudal dimension. The mass exhibited areas of mixed high attenuation, suggestive of hemorrhagic content. It was found to be communicating with soft tissue thickening in the third part of the duodenum, which was inseparable from the head of the pancreas. Accompanied by surrounding inflammation, mild free fluid, and resultant upstream fluid-filled dilation of the stomach, pylorus, and proximal duodenum, indicating an upper gastrointestinal obstruction (Fig. 1). Additionally, there was a hiatal hernia containing part of the gastric fundus, which showed wall thickening and surrounding free fluid, raising concerns for early congestion. Esophagogastroduodenoscopy (EGD) demonstrated severe esophagitis and cardia incompetence with a 3-cm hiatus hernia.
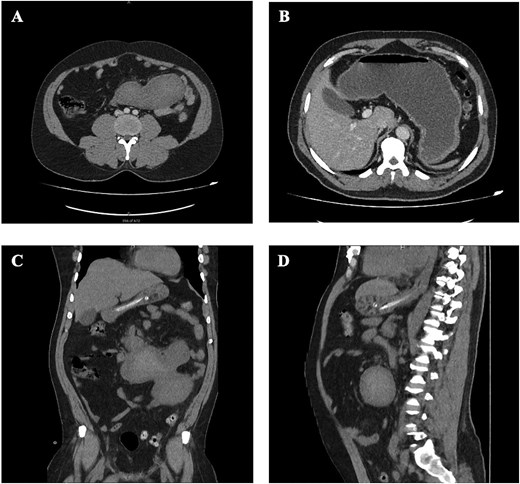
CT finding. (A, B) CT scan of abdomen, axial view. Showing an intra-abdominal large, lobulated mass, with internal mixed high attenuation, suggestive of hemorrhagic content. With resultant dilatation of the stomach and proximal duodenum. (C) CT scan of abdomen, coronal view. (D) CT scan of abdomen, sagittal view.
The patient underwent an exploratory laparotomy. Intraoperatively, a hemorrhagic mesenteric cyst was found in the small bowel mesentery, originating at the duodenojejunal (DJ) junction and measuring ~15 × 20 cm. The bowel wall was intact, the mesentery was viable, and there was no active bleeding (Fig. 2). Postoperative histopathology revealed a cyst with a fibro-adipose tissue wall, filled with granulation tissue and hemorrhage, confirming the diagnosis. The postoperative course was uneventful.

Intraoperative picture. Shows a large mass originating from the small bowel mesentery at the duodenojejunal (DJ) junction.
Discussion
Mesenteric cysts are rare, benign tumors found inside the abdomen, with an incidence rate of ~1 in 100 000–250 000 hospital admissions [5]. They can develop anywhere in the gastrointestinal mesentery, but they are most commonly seen in the small bowel mesentery (60%), followed by the large bowel mesentery (24%) and the retroperitoneum (14.5%) [1]. The exact cause of these cysts isn’t fully understood, but it’s thought that they might be linked to congenital malformations in the lymphatic channels, trauma, infections, or even changes in the mesenteric lymphatic tissue [5, 6]. Although many mesenteric cysts are asymptomatic, they may present with abdominal pain, abdominal distention, nausea, vomiting, and constipation. According to a review by Tan et al., abdominal pain was the most commonly reported symptom, which was seen in 63% of cases, while a palpable mass was found in 44% [6].
While it’s rare, hemorrhagic changes in mesenteric cysts have been noted, especially in larger cysts or those linked to trauma [3]. CT scans are typically the best way to diagnose these cysts because they can show the internal bleeding and any mass effects. Magnetic Resonance Imaging (MRI) could also be useful for spotting hemorrhagic elements and septations in cysts that are lymphangiomatous in nature [7]. In our patient, the CT scan showed a lobulated cystic mass with high-attenuation areas, which indicated hemorrhagic content, and it was compressing the third part of the duodenum.
The standard treatment of mesenteric cysts is surgical excision. Whether surgery is a laparotomy or done laparoscopically depends on factors like cyst size, location, and complications. For our patient, a laparotomy was necessary because of the cyst’s size and its obstructive effects. Removing the entire cyst is essential to avoid recurrence and to ensure a histological diagnosis [4]. While rare, malignant transformation into cystadenocarcinoma has been reported, making total excision of even asymptomatic cysts critical [8]. In our patient’s case, the histopathology report confirmed that the cyst was benign and hemorrhagic.
In conclusion, this case highlights the importance of considering hemorrhagic mesenteric cysts in the differential diagnosis of abdominal pain and intestinal obstruction. Imaging plays a key role in the diagnosis, and complete surgical excision remains the definitive treatment to prevent recurrence and rule out malignancy.
Conflict of interest statement
None of the authors has any conflicts of interest to disclose concerning this article.
Funding
None declared.



