-
PDF
- Split View
-
Views
-
Cite
Cite
Shawn T. Steen, Evan D. Slater, Casey E. Barbaro, Emma R. Huebner, An unexpected finding of hepatic lymphoma after emergent cholecystectomy, Journal of Surgical Case Reports, Volume 2017, Issue 3, March 2017, rjx051, https://doi.org/10.1093/jscr/rjx051
Close - Share Icon Share
Abstract
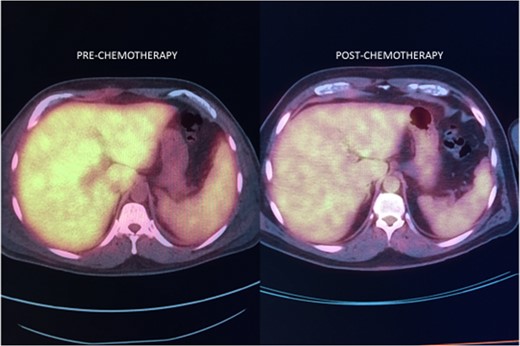
Herein we describe a case report of a patient with elevated liver enzymes, leukocytosis, anemia and fevers after cholecystectomy surgery done for presumed acute cholecystitis. Numerous post-surgical tests showed no acute surgical complications to account for the laboratory abnormalities. Due to systemic symptoms of joint pain and the chronicity of the symptoms, a liver biopsy was recommended by the gastroenterology service to rule out infectious or auto-immune causes. After the liver biopsy, the patient was diagnosed with intravascular large B-cell lymphoma (IVLBCL), a subset of diffuse large B-cell lymphoma. After a thorough lymphoma evaluation, the IVLBCL was found to be isolated to the liver and treated successfully with chemotherapy. This is only the second case report in the literature of this entity.
INTRODUCTION
We present a case of intravascular large B-cell lymphoma (IVLBCL) located solely within the liver. IVLBCL isolated to the liver is extremely rare. This posed a diagnostic dilemma for the treating team as the diagnosis was made after cholecystectomy surgery with persistent elevated liver enzymes, leukocytosis, fevers and anemia.
CASE REPORT

Intra-operative cholangiogram showing good flow of bile into duodenum.
DISCUSSION
We present a rare case of IVLBCL isolated to the liver. IVLBCL, a subset of diffuse large B-cell lymphoma, is the intravascular proliferation of clonal lymphocytes with little to no involvement of the organ parenchyma. Lymphoma cells are not present in the lymph nodes. This causes a lack of the typical lymphadenopathy found in most lymphomas. Treatment typically mirrors that of the more common lymphoma types. Most of the information available on this rare lymphoma has been collected from individual case reports over several decades.
IVLBCL has been described in the small vessels of nearly every organ, often with difficult initial diagnoses. Previous case reports describe IVLBCL presenting as interstitial lung disease, adrenal failure, pulmonary hypertension, nephrotic syndrome, myocardial infarction and polyarthritis. IVLBCL may be grouped into several discrete presentations, however, including CNS involvement, cutaneous involvement, fever of unknown origin and hemophagocytic syndrome [1–3]. An accurate and timely diagnosis is difficult due to a common lack of significant adenopathy, hepatosplenomegaly or circulating cells in the peripheral blood [1]. Serum laboratories may assist in the diagnosis. Increased serum LDH and β2-microglobulin levels are observed in greater than 80% of IVLBCL patients, elevated erythrocyte sedimentation rate (ESR) in 43%, and altered hepatic, renal or thyroid function tests in 15–20% [4]. Our patient exhibited increased β2-microglobulin levels as well as elevated ESR with transaminitis.
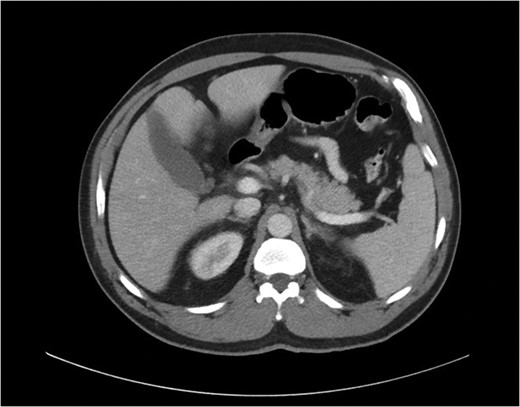
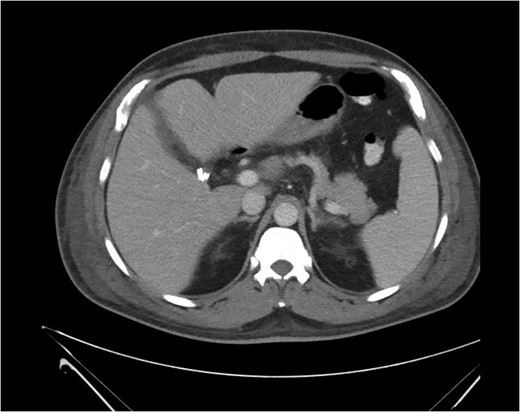
Biopsy of the affected organ is the only way to confirm the diagnosis of intravascular lymphoma. The predominant microscopic finding of IVLBCL is atypical blastoid cells with multiple mitoses that exclusively proliferate within vascular and sinusoidal structures of the organ. Mouse xenograft models have indicated that inhibition of cell migration may be involved in IVLBCL pathogenesis and may account for the limited growth locations within the host [5]. Immunohistochemical staining is positive for B-cell markers CD19, CD20, CD22 and CD79a in the absence of staining for T-cell markers [1, 6, 7]. On imaging, both primary and secondary hepatic lymphomas show mild enhancement after contrast administration including a homogeneous and rim-like pattern, and central necrosis may produce a heterogeneous appearance. Most patients with primary or secondary hepatic lymphomas also present with associated lymphadenopathy, whereas patients with IVLBCL frequently have neither central necrosis nor lymphadenopathy, presentations that may aid in differential diagnosis of IVLBCL from other forms of hepatic lymphomas [7].
Noncutaneous IVLBCL in particular is normally associated with poor long-term prognosis. In most cases, IVLBCL is disseminated at the time of diagnosis, warranting treatment with systemic therapy [1]. Successful IVLBCL treatment has been achieved with modified R-VNCOP-B (etoposide, mitoxantrone, cyclophosphamide, vincristine, prednisolone and bleomycin plus rituximab) regimen [2]. R-CHOP therapy, utilized in combination with high-dose methotrexate therapy as prophylactic CNS coverage, has also been successful in other IVLBCL cases with hepatic involvement [3, 7].
There is only one other case report in the literature describing IVLBCL isolated to the liver and the patient had a similar constellation of symptoms to ours [7]. Most reports of IVLBCL cases share similar presentations: prolonged fevers, elevated liver enzyme levels, hyperbilirubinemia and elevated LDH levels [8, 9]. A reported severe variant of IVLBCL includes multiorgan failure, pancytopenia and hemophagocytic syndrome [10, 11]. As outlined in our report, elevated liver function tests, leukocytosis and fevers caused significant concern for post-operative complications after a routine gallbladder surgery. In the end, the findings were all due to an underlying pathology unrelated to surgical gallbladder disease.
CONCLUSIONS
In conclusion, this study describes a unique presentation of hepatic involvement of IVLBCL and supports the utilization of random liver biopsy in a patient who presents with fever of unknown origin and elevated liver enzyme levels, among other symptoms. Awareness of the heterogeneous presentations of IVLBCL is important in order for a timely diagnosis to be made that allows for effective systemic therapy.
CONFLICT OF INTEREST STATEMENT
None declared.



