-
PDF
- Split View
-
Views
-
Cite
Cite
Hugo Meunier, Benjamin Menahem, Andrea Mulliri, Audrey Fohlen, Nicolas Contival, Yannick Le Roux, Julien Desgue, Jean Lubrano, Arnaud Alves, Esophagopericardial fistula: an unexpected dreaded complication of treatment of leak following revisional sleeve gastrectomy by endoscopic internal drainage, Journal of Surgical Case Reports, Volume 2017, Issue 3, March 2017, rjx049, https://doi.org/10.1093/jscr/rjx049
Close - Share Icon Share
Abstract
Esophagopericardial fistula (EPF) is an uncommon but life-threatening complication of upper gastrointestinal tract surgery or endoscopy, which is related to anastomotic breakdown, chronic infection or esophageal traumatism. We first describe the first case of an EPF secondary to double pigtail drain migration: an endoscopic internal approach for the treatment of leak following revisional sleeve gastrectomy.
INTRODUCTION
The rapid increase in the number of bariatric surgeries such as sleeve gastrectomy (SG) or Roux-en-Y gastric bypass has driven a parallel increase in revisional bariatric surgeries which is needed in 5–50% of patients [1, 2]. Leaks remain a major complication after primary SG, due to its associated high morbidity and mortality [3, 4]. According to a recent review comparing primary and revisional SG, rates of leak, complication and re-operations were higher after revisional SG [5]. Management of leaks after SG is challenging and more complex, including surgical revision, percutaneous drainage of abcess, enteral hyper-alimentation and antibiotics therapy [6–9]. Endoscopic approach developed recently using deployment of stents or pigtail drain [8, 9]. However, pigtail drain acts as a foreigner body, which can migrate through fluid collection. We reported the first case of esophagopericardial fistula (EPF) secondary to migration of a double pigtail drain, set up in order to resolve a gastric leak after revisional SG.
CASE REPORT
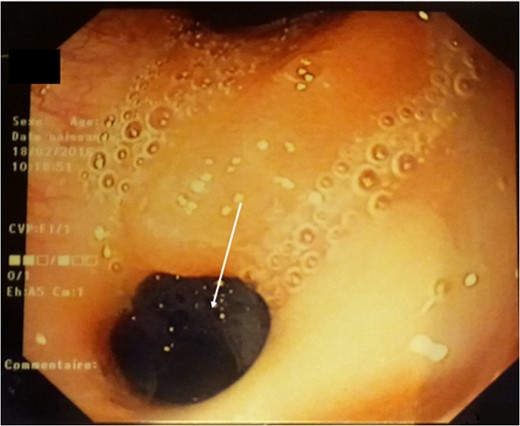
Fibroscopy: a 5-mm fistulous hole on the high part of the stomach.

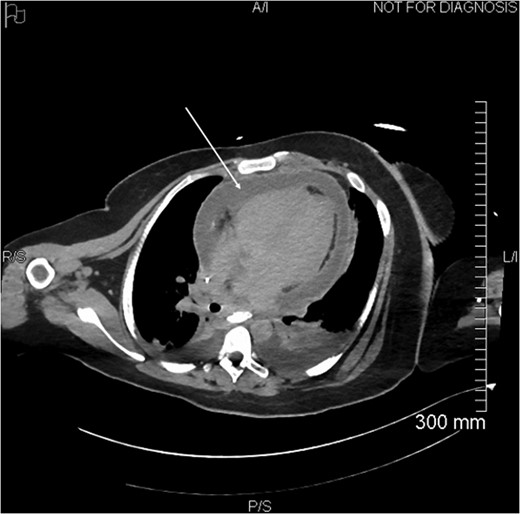
Control X-ray after the double pigtailed drain has been put up.
Proximal end of the double pigtail drain externalizes in the pericardium (arrow).
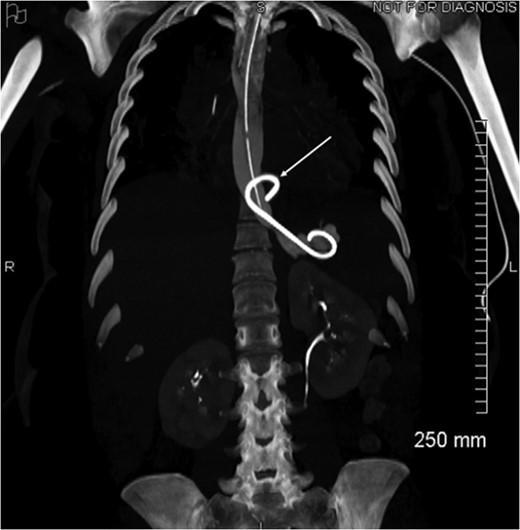
Coronal view of opacification on CT showing the externalization of the drain in the pericardium (arrow).
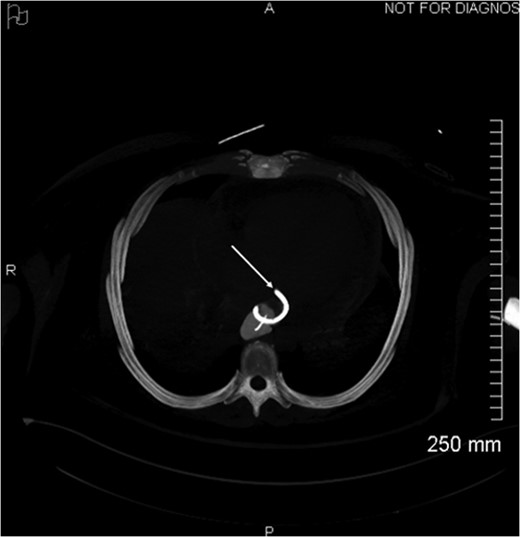
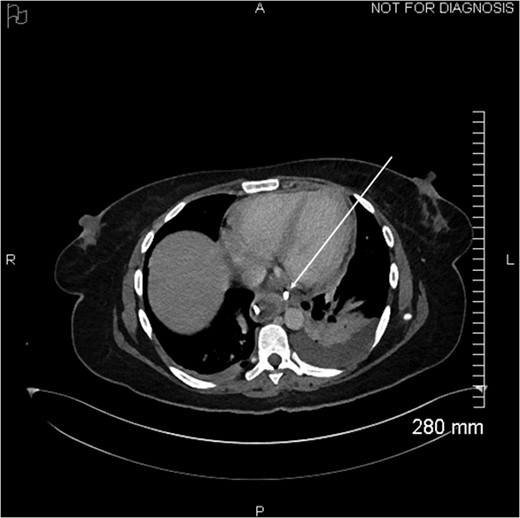
Axial view of opacification on CT showing the externalization of the drain in the pericardium (arrow).
CONFLICT OF INTEREST STATEMENT
None declared.
ACKNOWLEDGMENTS
None.



