-
PDF
- Split View
-
Views
-
Cite
Cite
Nese Keser, Erhan Celikoglu, İmam H. Aydın, Nurver Ozbay, The outcome of a pregnant woman with a minor head injury: an ossified subdural hematoma (OSDH), Journal of Surgical Case Reports, Volume 2017, Issue 3, March 2017, rjx048, https://doi.org/10.1093/jscr/rjx048
Close - Share Icon Share
Abstract
We experienced an ossified subdural hematoma (OSDH), which is an extremely rare form of chronic subdural hematoma (SDH), in the dominant hemisphere of a 35-year-old woman. She presented to our outpatient clinic with a complaint of a headache; she had previously experienced a head injury while she was pregnant. We performed surgery with extreme caution because the lesion was attached to the surrounding tissue. Since an OSDH is an extremely rare form of chronic SDH, neurosurgeons might not experienced them during their daily practice. Additionally, head injuries received during pregnancy should be taken seriously, and after delivery, the patient should undergo cranial computed tomography, even if she is asymptomatic.
INTRODUCTION
A chronic subdural hematoma (SDH) is a well-known complication following head injury. The incidence of calcification identified radiologically in the membrane of a chronic SDH is 0.3–2.7% [1, 2]. Calcification is more prominent in children and young adults than it is in elderly patients [3].
Calcified SDHs are relatively frequent, but an ossified SDH (OSDH) is extremely rare [1, 4, 5]. It is difficult to decide whether to operate on patients with OSDHs since the lesions often adhere to brain tissue, thereby increasing operative risks [2]. We observed such a mass in the dominant hemisphere of a 35-year-old woman. She had no complaints other than a headache and was free of deficits, as confirmed by a neurological examination. Since operation is recommended in symptomatic patients, we performed surgery due to the patient's reported headache.
CASE REPORT
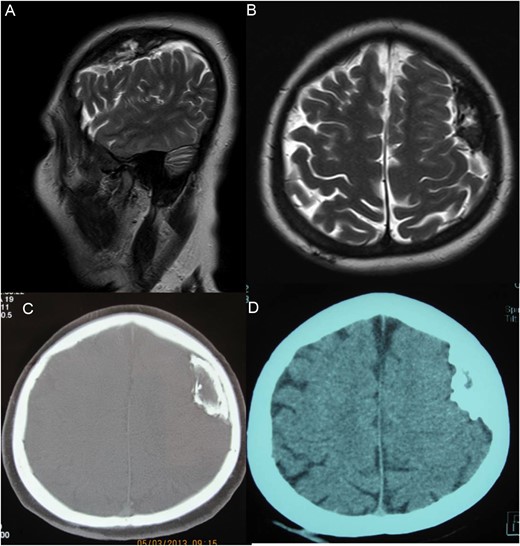
Cranial magnetic resonance (MR) and cranial CT images from a woman with an OSDH. (A) Pre-operative sagittal and axial (B) T2-weighted MR images demonstrating an ossified subdural mass in the left frontoparietal region. Pre-operative CT scan showing bone (C) and brain matter (D) of the ossified subdural mass that was located in the left frontoparietal region. Note that the mass has outer and inner rims and a slightly hypodense central part.
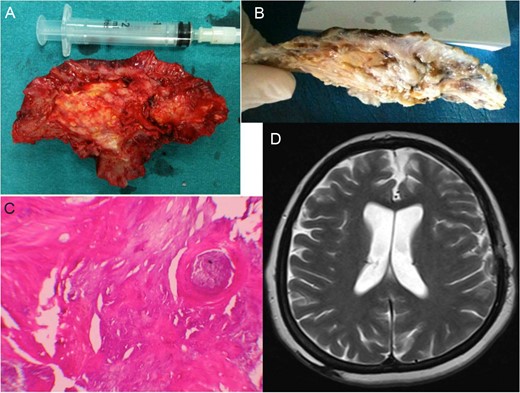
The peri-operative macroscopic appearance of the OSDH (A). Macroscopic appearance of the OSDH after formaldehyde fixation (B). Microscopic examination of the specimen stained with hematoxylin and eosin, original magnification ×100. In addition to the calcification areas, there is an area of irregular ossification with trabeculation (C). Six months after the operation: axial T2-weighted magnetic resonance images of the patient are normal (D).
DISCUSSION
Chronic SDH, which is a well-known complication following head injury, has frequently been reported. McKissock et al.[6] reported this condition 21 days following an injury. Chronic SDHs generally occur in individuals who are 50–60 years of age and in 50–75% of cases in which there is a history of head injury. The most apparent symptom of chronic SDH is a headache followed by lethargy, confusion, memory impairment and epilepsy. Motor deficits present as hemiparesis or gait abnormalities [6].
The next phase in chronic SDH is calcification, which occurs after a minimum of 6 months [1, 7, 8]. The degree of calcification extends from a mild calcified inner membrane to gross calcification and even ossification of the hematoma. The pathogenesis of this calcification is not clearly understood. Vascular, metabolic and local factors are thought to play a role in calcification [7], as unilateral calcification may occur in some bilateral SDHs. Afra [7] attributed circulation in the subdural region with absorption and vascular thrombosis as causative local factors. The most frequent complaint among patients with calcified SDH is a headache [9], especially in young patients who are more affected by intracranial pressure [10].
In most cases, diagnosis is made by MRI and CT; however, in some cases, operative findings and pathological examinations are required.
Terminal-phase ossification [8] is less common than calcification is in SDH. The pathogenesis of OSDH is also not clearly understood. However, tissue irritation from calcification has been attributed to causing ossification that may occur years later [1, 7]. Symptoms of OSDH may include epilepsy, dysphasia, hemiparesis, gait abnormalities and mental retardation [1, 8]. However, most cases are completely asymptomatic [2]. In our patient, the symptom was a headache, in contrast to findings reported in the literature. Since surgery was indicated for symptomatic patients, she underwent surgery.
During the operation, extreme caution should be used during dissection since the lesion may be attached to the surrounding tissue [2]. In our case, a definitive diagnosis was made based on the pathology results (Fig. 2C).
Full postoperative recoveries have been reported following symptomatic OSDHs [1, 8, 9]. Similar to these reports, our patient was free of headaches and asymptomatic after surgery.
Due to our experience with this case, since OSDHs may be asymptomatic, we suggest that even mild head injuries received during pregnancy should be taken seriously; we emphasize the necessity of cranial CT after labor.
We encountering patients with ossified lesions detected by MRI or CT, physicians should remember that the lesion might be an OSDH and attached to the surrounding tissue, so extreme caution must be used during excision to ensure a successful operation.
FUNDING
None.
ACKNOWLEDGEMENT
We would like to thank Editage (www.editage.com) for English language editing.
CONFLICT OF INTEREST STATEMENT
None declared.



