-
PDF
- Split View
-
Views
-
Cite
Cite
Justin M. Hintze, Donal B. O'Connor, Peter Molony, Paul C. Neary, Distant melanoma causing small bowel obstruction, Journal of Surgical Case Reports, Volume 2017, Issue 2, February 2017, rjx020, https://doi.org/10.1093/jscr/rjx020
Close - Share Icon Share
Abstract
Small bowel obstructions (SBOs) are common. Adhesions make up the majority of cases at 84.9%, followed by abdominal herniae and malignancies. A 71-year-old female presented with total constipation, abdominal distension, on a background of resected cutaneous melanoma nine years prior. A CT-scan showed small bowel intussusception and disseminated mucosal-enhancing lesions consistent with metastases. She was brought to the operating theatre where six areas of intussusception were identified and manually reduced. Biopsies confirmed the diagnosis of melanoma. Melanoma of the gastrointestinal tract (GIT) is rare, with most cases occurring as metastasis from cutaneous lesions. Melanomas of the GIT are usually asymptomatic in their early stages, and are often diagnosed when complications, such as obstruction or perforation occur. Management of such cases consists mainly of surgical intervention to resolve the complication. In people who present with SBO without previous surgeries or herniae, a malignant cause must be considered.
INTRODUCTION
Small bowel obstructions (SBOs) are common, making up 15% of all acute surgical admissions [1]. Post-operative adhesions make up the majority of cases at 84.9%, followed by abdominal herniae in 3.3% and malignant tumours in 2.5% [2]. Small bowel malignancies only account for 5% of all gastrointestinal malignancies, of which 44% are carcinoid tumours, 33% are adenocarcinomas, 17% are stromal tumours and 8% lymphomas [3]. Carcinoid tumours have a predilection for involving the ileum, whereas adenocarcinomas usually occur in the duodenum and stromal tumours in the jejunum.
Metastatic melanoma to the small bowel is rare, but a malignant cause of SBO should be considered in cases where no previous surgeries or herniae can be identified.
CASE PRESENTATION
A 71-year-old female presented to the emergency department with constipation and obstipation for the previous 3 days. Associated with that she had nausea and vomiting.
Her past medical history included type 2 diabetes mellitus. Her surgical history was significant for a primary cutaneous melanoma excision on her right arm 9 years prior to her presentation. She had attended routine follow-up for 5 years following her melanoma surgery.
On initial examination she had clinical signs of dehydration—dry mucous membranes, oliguria, decreased skin turgor—a grossly distended abdomen, no abdominal scars or herniae and high-pitched bowel sounds.

Coronal CT showing small bowel to small bowel intussusception (arrow).
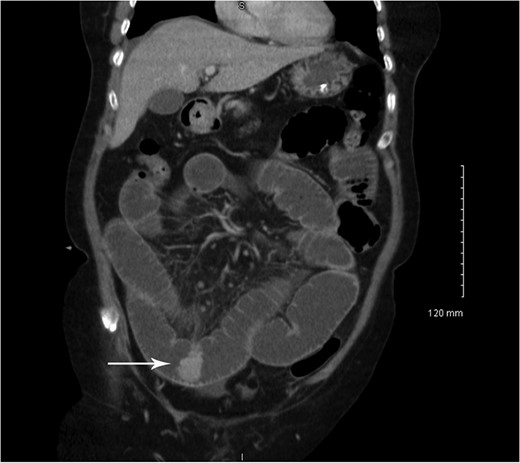
Coronal CT showing small bowel mucosal-enhancing lesion (arrow).

Intra-operative picture demonstrating one area of small bowel to small bowel intussusception.
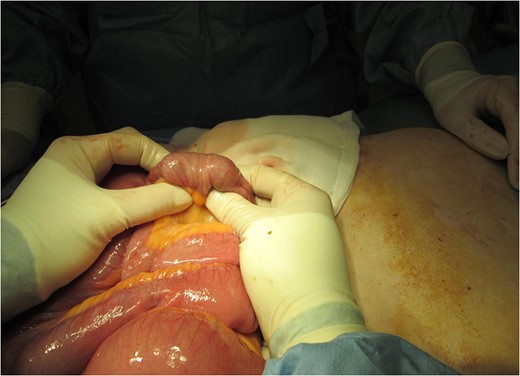
Intra-operative picture demonstrating the same area of small bowel to small bowel intussusception post manual reduction.
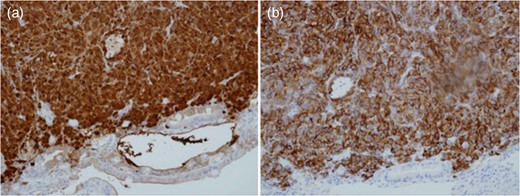
Biopsy of intestinal lead-point for intussusception demonstrating positivity for S100 (a) and melan-A (b).
Subsequent staging CT demonstrated brain and lung metastasis. The patient was commenced on systemic chemotherapy, in addition to a low-residue diet and did not require any further intervention for bowel obstruction. She died 9 months later from metastatic disease.
DISCUSSION
Melanoma of the gastrointestinal tract (GIT) is relatively rare, with most cases occurring as metastasis from cutaneous primary lesions [4]. In one study up to 60% of all patients with melanoma had intestinal metastasis at autopsy, with the small intestine being involved in 50%, the colon in 31% and the anorectum in 25% of cases. Overall, melanoma accounts for 1–3% of all GI malignancies [5], with most of these being metastatic lesions. Only 24 cases of primary melanoma of the small bowel have been reported in the literature to date [6]. However, in up to 26% of cases of intestinal melanomas, no extra-intestinal primary lesion can be identified [7]. In such circumstances, spontaneous regression of the primary site may explain the lack of a primary melanoma. Among intestinal malignancies, metastatic melanoma is the fifth most common malignancy, however is considered to be the extra-intestinal malignancy most likely to metastasize to the GIT. The most common site is the small intestine, owing to the rich blood supply [8]. Melanomas of the GIT are usually asymptomatic in their early stages, and are often diagnosed when acute and sometimes life-threatening complications, such as obstruction, perforation or haemorrhage occur [4]. The most common presentation of small intestinal melanoma is obstruction secondary to intussusception [4]. While intussusception is the second most common cause of acute abdominal emergency in children, it only causes between 1 and 5% of all obstructions in adults. The most frequent site in adults is the small bowel, followed closely by the ileocaecal area.
Management of such cases consists mainly of surgical intervention to resolve the acute obstruction/intussusception and stabilizing the patient. In cases where metastatic disease is limited to one or a very limited number of enteric metastasis, a metastatectomy can be considered. If an R0-status cannot be achieved or there is recurrent disease, systemic therapy with immunotherapy, chemotherapy or molecular targeted therapy, such as Vemurafenib, Ipilimumab, Pembrolizumab or Imatinib, can be considered, depending on performance status and positivity for BRAF and KIT [9]. Late recurrences of melanoma, defined as a disease-free interval of at least 10 years, have been reported as occurring in 1–25% of cases [10].
SBOs are common surgical emergencies, accounting for 15% of all acute surgical admissions. In people who present with SBO without previous surgeries or obvious herniae, a malignant cause must be considered. Melanoma is the most common extra-intestinal malignancy to metastasize to the GIT and metastases can occur many years later.
ACKNOWLEDGEMENT
The authors would like to thank the patient and their family for allowing this case and images to be used in this case report.
CONFLICT OF INTEREST STATEMENT
None of the contributing authors have any conflicts of interest to disclose.
REFERENCES
- small bowel obstruction
- computed tomography
- biopsy
- cancer
- constipation
- adhesions
- intestine, small
- intussusception
- melanoma
- neoplasm metastasis
- operating room
- surgical procedures, operative
- abdomen
- diagnosis
- mucous membrane
- skin lesion
- gastrointestinal tract
- abdominal swelling
- malignant melanoma, cutaneous



