-
PDF
- Split View
-
Views
-
Cite
Cite
Marios S. Themistocleous, Elias Antoniades, Dimitrios Giakoumettis, Aristoteles V. Kalyvas, Andreas Mitsios, George Sfakianos, Herpes simplex virus Type 1 encephalitis in an adolescent presenting with acute hydrocephalus, Journal of Surgical Case Reports, Volume 2017, Issue 2, February 2017, rjx013, https://doi.org/10.1093/jscr/rjx013
Close - Share Icon Share
Abstract
Herpes simplex virus Type 1 (HSV-1) is a human neurotropic virus causing encephalitis, corneal blindness or several peripheral nervous system disorders. Herpes Simplex encephalitis (HSE) is the most devastating clinical syndrome with severe morbidity and mortality. Hydrocephalus associated with viral meningoencephalitis is an extremely rare entity with only few documented cases, predominantly due to HSV-2 infection. HSV-1 infection of central nervous system present in the majority of the cases as encephalitis. We report a rare case of an 11-year-old child suffering from HSV-1 infection of central nervous system causing hydrocephalus without evidence of encephalitis.
INTRODUCTION
Viral meningoencephalitis leading to hydrocephalus is an extremely rare entity with only few documented cases, predominantly due to HSV-2 infection. Herpes simplex virus Type 1 (HSV-1) infection of central nervous system present in the majority of the cases as encephalitis. We report a case of HSV-1 encephalitis without clinical signs presenting with occlusive hydrocephalus.
CASE REPORT
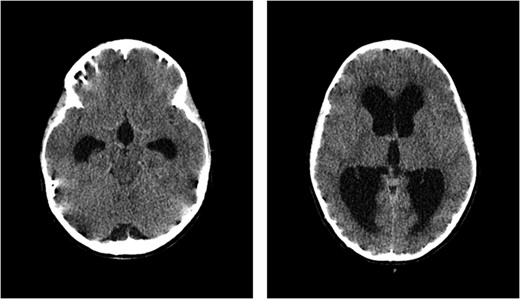
CT scan of the brain showed acute hydrocephalus with massive dilatation of lateral and third ventricles (at mesencephalon and thalamus levels, respectively).
An external ventricular drain was placed. Cerebrospinal fluid analysis of the intraoperative sample revealed 27 cells/μl, with <20 mg/dl glucose and 61 mg/dl albumin concentration, respectively. Gram-stain and culture were negative for bacteria. Moreover, cerebral spinal fluid (CSF) was sent for polymerase chain reaction (PCR) examination of HSV-1,-2, Varicella zoster Virus, Enteroviruses, West Nile and Dengue viruses. The results were positive for HSV-1.
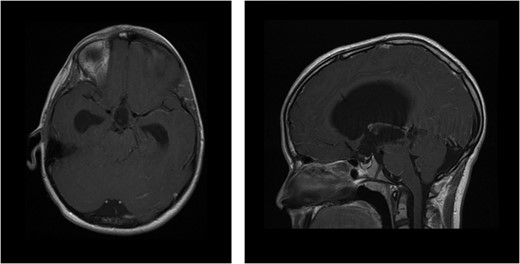
MRI of brain enhanced with contrast agent showing ventricular dilatation with aqueducts occlusion (axial and sagittal sequences, respectively).
| . | Day 0 . | First post-op. day . | Fifth post-op. day . | Eighth post-op. day . | 12th post-op. day . | 17th post-op. day . | 22nd post-op. day . |
|---|---|---|---|---|---|---|---|
| CSF | |||||||
| Cells | 27/μl | 5/μl | 5/μl | 10/μl | 12/μl | 2/μl | 0/μl |
| Glucose | <20 mg/dl | 68 mg/dl | 50 mg/dl | 57 mg/dl | 54 mg/dl | 60 mg/dl | 54 mg/dl |
| Albumin | 61 mg/dl | 48 mg/dl | <20 mg/dl | <20 mg/dl | 20 mg/dl | <20 mg/dl | <20 mg/dl |
| Gram-Stain | Negative | Negative | Negative | Negative | Negative | Negative | Negative |
| PCR | + for HSV1 |
| . | Day 0 . | First post-op. day . | Fifth post-op. day . | Eighth post-op. day . | 12th post-op. day . | 17th post-op. day . | 22nd post-op. day . |
|---|---|---|---|---|---|---|---|
| CSF | |||||||
| Cells | 27/μl | 5/μl | 5/μl | 10/μl | 12/μl | 2/μl | 0/μl |
| Glucose | <20 mg/dl | 68 mg/dl | 50 mg/dl | 57 mg/dl | 54 mg/dl | 60 mg/dl | 54 mg/dl |
| Albumin | 61 mg/dl | 48 mg/dl | <20 mg/dl | <20 mg/dl | 20 mg/dl | <20 mg/dl | <20 mg/dl |
| Gram-Stain | Negative | Negative | Negative | Negative | Negative | Negative | Negative |
| PCR | + for HSV1 |
| . | Day 0 . | First post-op. day . | Fifth post-op. day . | Eighth post-op. day . | 12th post-op. day . | 17th post-op. day . | 22nd post-op. day . |
|---|---|---|---|---|---|---|---|
| CSF | |||||||
| Cells | 27/μl | 5/μl | 5/μl | 10/μl | 12/μl | 2/μl | 0/μl |
| Glucose | <20 mg/dl | 68 mg/dl | 50 mg/dl | 57 mg/dl | 54 mg/dl | 60 mg/dl | 54 mg/dl |
| Albumin | 61 mg/dl | 48 mg/dl | <20 mg/dl | <20 mg/dl | 20 mg/dl | <20 mg/dl | <20 mg/dl |
| Gram-Stain | Negative | Negative | Negative | Negative | Negative | Negative | Negative |
| PCR | + for HSV1 |
| . | Day 0 . | First post-op. day . | Fifth post-op. day . | Eighth post-op. day . | 12th post-op. day . | 17th post-op. day . | 22nd post-op. day . |
|---|---|---|---|---|---|---|---|
| CSF | |||||||
| Cells | 27/μl | 5/μl | 5/μl | 10/μl | 12/μl | 2/μl | 0/μl |
| Glucose | <20 mg/dl | 68 mg/dl | 50 mg/dl | 57 mg/dl | 54 mg/dl | 60 mg/dl | 54 mg/dl |
| Albumin | 61 mg/dl | 48 mg/dl | <20 mg/dl | <20 mg/dl | 20 mg/dl | <20 mg/dl | <20 mg/dl |
| Gram-Stain | Negative | Negative | Negative | Negative | Negative | Negative | Negative |
| PCR | + for HSV1 |
DISCUSSION
Due to the fact that aqueduct is the narrowest segment of CSF pathway, it is the commonest site of intraventricular obstruction. Stenosis is responsible for 6–66% of cases of pediatric hydrocephalus. There are two peaks of distribution of age, one in the first year of life and the second in adolescence [1]. Aqueductal stenosis is not to be considered a stable condition. Often it may be tolerated for years [2] in a condition described by Oi et al. [3] as arrested hydrocephalus used for patients who may harbor an undetected stenosis. To these mechanisms accounted a partially occluded aqueduct, employment of alternative CSF pathways and alteration in CSF production [3]. It is also suggested that head injuries, subarachnoid hemorrhages or viral infections may worsen the occlusion [4].
In viral infections, the mechanism is attributed either to an ependymitis leading to desquamation of ependyma with subsequent mechanical obstruction [5] or to a cross linking between ependymal cells caused by viral particles bridges [6]. At the aqueduct location, where continuous CSF bathing with released viruses takes place, the high accumulation of particles promotes this process [6]. In addition to that the pathological findings and subsequently the radiological ones do not prove a gliosis compared to the bacterial infections [1].
The majority of the documented cases of viral infection and hydrocephalus development are mostly attributed to HSV-2 infection, which causes usually meningitis and shows a more benign course compared with the HSV-1 [7]. One characteristic case of HSV-1 encephalitis and hydrocephalus was described by Tyagi et al. [8].
Due to the infection presence [9] and the prolonged hospitalization period of the child who might be burdened with a potential reoperation of stoma obstruction after a third ventriculo-stomy, the ventriculo-peritoneal shunt implantation was preferred.
Epitomizing the aforementioned issues, it could be concluded that by the presence of hydrocephalus without a gross obstructing intracranial lesion the suspicion of subclinically manifested viral encephalitis should be raised and thus the PCR for HSV-1 should also be included in the diagnostic tests as well, defining on the same time the optimal surgical treatment.
CONFLICT OF INTEREST STATEMENT
The authors report no conflicts of interest.



