-
PDF
- Split View
-
Views
-
Cite
Cite
Nabil M. Nuamah, Cem Ibis, Ali F.K. Gok, Feza Ekiz, Bulent Acunas, Duplicated common bile duct: a recipe for biliary injury. Report of a new variant, Journal of Surgical Case Reports, Volume 2017, Issue 2, February 2017, rjx021, https://doi.org/10.1093/jscr/rjx021
Close - Share Icon Share
Abstract
Duplicated common bile duct, often associated with conditions like lithiasis, biliary cysts and pancreatobiliary maljunction, could result in highly morbid and potentially fatal biliary injuries. Precise preoperative diagnosis and classification still remain a challenge. A female patient undergoing emergency laparoscopic cholecystectomy for acute calculous cholecystitis sustained iatrogenic bile duct injury. A drainage tube was placed into the injured duct for post-operative conservative management. Post-operative tube cholangiogram revealed a double common bile duct with cystic duct opening distally. This was identified as a new variant not previously reported or classified. However rare, duplicated common bile duct could result in serious iatrogenic bile duct injury if unidentified during surgery. Knowledge of its existence is essential to avoid such injuries as preoperative diagnosis still remains a challenge. A thorough clinical and morphological study of previously reported variants is needed for a comprehensive classification to encompass newly discovered variants.
INTRODUCTION
Extrahepatic biliary duct duplication, also commonly called duplicated common bile duct (DCBD), is exceptionally rare and mostly turn to be unexpected finding during surgery exposing surgeons to unusual surprises leading to iatrogenic bile duct injuries (BDI). This anomaly has been reported to be associated with multiple disorders including cholelithiasis, choledocholithiasis, choledochal cyst, pancreatobiliary maljunction (PBM) and malignancy [1]. Recognition of the existence of this anomaly is important to prevent iatrogenic biliary injury and most importantly help in making the right surgical decision. After the first case of DCBD reported by Vesalius in 1543, numerous cases of different variants have been reported in the English literature across the globe [2–5]. Only seven out of nine variants currently described in the literature can be classified by available classification systems [4]. Presented here-in, is a new variant of DCBD discovered after iatrogenic bile duct injury during laparoscopic cholecystectomy. The importance of recognition of its existence to avoidance BDI during surgery coupled with the need for a comprehensive classification system to encompass newly discovered variants are highlighted.
CASE PRESENTATION
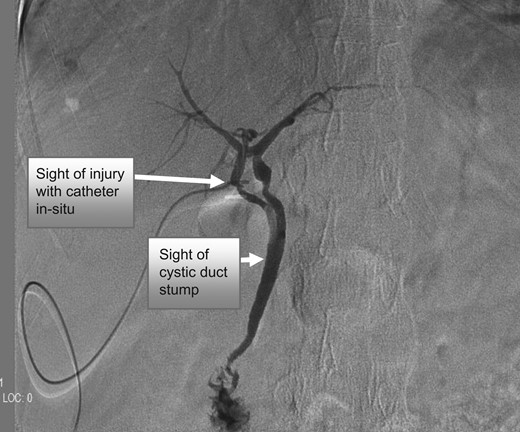
Cholangiogram showing the double duct originating from the hepatic hilus with injury on the right duct. The two ducts drain singly with cystic duct opening into the common duct.
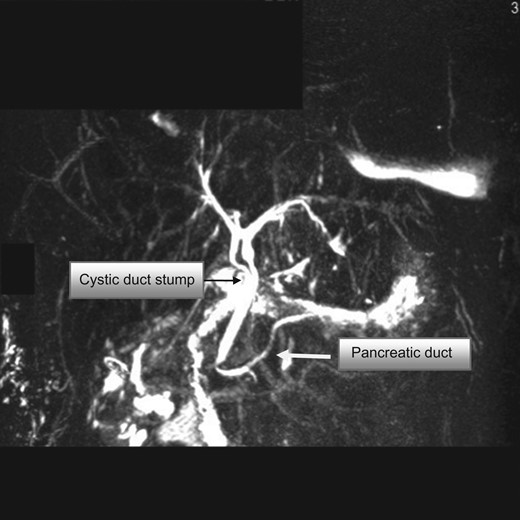
MRCP showing the double common bile duct, cystic duct stump and pancreatic duct. The cystic duct stump is noted to open distally into the common duct.
DISCUSSION
![Modified double common bile duct classification proposed by Choi et al. Type I: CBD separated by septum; Type II: CBD that bifurcates to drain separately; Type III: double biliary drainage without extrahepatic communication channels (without [IIIa] or with [IIIb] intrahepatic connecting channels); Type IV: double biliary drainage with one or more extrahepatic communication channels; Type V: single biliary drainage of double extrahepatic bile ducts without (Va) or with (Vb) communication channels.](https://oupdevcdn.silverchair-staging.com/oup/backfile/Content_public/Journal/jscr/2017/2/10.1093_jscr_rjx021/11/m_rjx021f03.jpeg?Expires=1775503024&Signature=aFC2b1-Jpl1meKGR0fuc-MWz5tuX9ajcboLHmAeVNslpPGEDcLzYvaF2NagK3Bf2q-c66c48kBcHE~r8lEfiDeMnhUWwiXg8uNvOXNoPU6VsqTIPMKFTstPTzi0p5nSoVTaK23uEvSRTtrpKG17b7SxZ5yyjLJ0dMPS4p~~BRKM8Ex0zhFeF8tDatKdPpY5xb5zA0vq1IUNTygFNPo0sh5KsuC7sD-1dbijFY1VgAr0Ns77yklUIFe1aoT7C1L5ypTr0HH4JjljsBPEsttmPdjtkoXZ~Wu9U0seA6lyotspW4DvuaEwMq58jEWn3SeVVAKxzXXXJMnooBhpnoQ6YHQ__&Key-Pair-Id=APKAIYYTVHKX7JZB5EAA)
Modified double common bile duct classification proposed by Choi et al. Type I: CBD separated by septum; Type II: CBD that bifurcates to drain separately; Type III: double biliary drainage without extrahepatic communication channels (without [IIIa] or with [IIIb] intrahepatic connecting channels); Type IV: double biliary drainage with one or more extrahepatic communication channels; Type V: single biliary drainage of double extrahepatic bile ducts without (Va) or with (Vb) communication channels.

Unclassified reported variants. (A) Variant described by Paraskevas et al. and Sahu et al.(B) Variant described by Kosar et al.(C) Variant described in current report.
CONCLUSION
Extrahepatic bile duct duplication could be a recipe for disaster during surgery and a prior knowledge of its existence is important to avoid inadvertent BDI. A thorough review of all reported variants is needed for a comprehensive classification system of clinical significance.
ACKNOWLEDGEMENTS
We thank Dr Jared A. White (UAB liver transplant and hepatobiliary surgery, Birmingham, USA) and Dr G. Paraskevas of Greece for responding to our request seeking some clarification on their publication.
DISCLOSURE
Non-financial support disclosed.
COMPETING INTERESTS
None declared.



