-
PDF
- Split View
-
Views
-
Cite
Cite
Brett Sydney Bernstein, Rory George Callan, Darryl Ethan Bernstein, Tom Pampiglione, Hepatic portal venous gas: acute deterioration in an elderly patient, Journal of Surgical Case Reports, Volume 2017, Issue 12, December 2017, rjx245, https://doi.org/10.1093/jscr/rjx245
Close - Share Icon Share
Abstract
A 91-year-old female presented to the Emergency Department with a 10-day history of constipation and abdominal pain. Abdominal examination was normal and rectal examination showed faecal loading. A phosphate enema was given and the patient was admitted. Overnight, the patient’s GCS dropped from 15/15 to 3/15 and an arterial blood gas showed a lactate of 8 mmol/L (1.5 on admission). Abdomen remained soft throughout. A CT scan showed a large amount of free air and free fluid within the abdomen and pelvis, highly suspicious for perforation. Hepatic portal venous gas (HPVG) was visible, with portal venous air fluid levels noted. The patient was treated palliatively and died shortly thereafter. HPVG is a recognized but rarely identified radiological sign, which is a poor prognostic indicator, with most cases subsequently proving terminal, often due to subsequent bowel necrosis.
CASE REPORT
A 91-year-old female patient presented to the emergency department with a 10-day history of constipation and abdominal pain. On examination she had a soft abdomen, with mild left sided abdominal tenderness. She was otherwise clinically stable with no other abnormal findings on physical examination. A rectal examination was performed which showed faecal loading. Her past medical history was of hypertension, type 2 diabetes mellitus, hypercholesterolaemia and chronic anaemia. Bloods on admission showed an elevated CRP (54.8 mg/L), but were otherwise unremarkable. An admission venous blood gas was performed, with a lactate of 1.5 mmol/L. An abdominal X-ray showed left sided faecal loading, but no obstruction. She was initially treated as constipation with a phosphate enema.
She remained clinically well, until early the following morning when she became hypotensive with a blood pressure of 84/50 mmHg, and her conscious level as recorded by the Glasgow Coma Scale (GCS) dropped significantly from 15/15 to 3/15. An arterial blood gas was performed—lactate had increased to 8 mmol/L. At this point her abdomen remained soft.
Subsequently a computerized tomography scan was performed of her chest, abdomen and pelvis (CTCAP), showing hepatic portal venous gas (HPVG), with visible air fluid levels (Fig. 1). There was a large amount of free air and free fluid within the abdomen and pelvis, highly suspicious for perforation (Fig. 2). There was also partial ischaemia of liver segment seven.
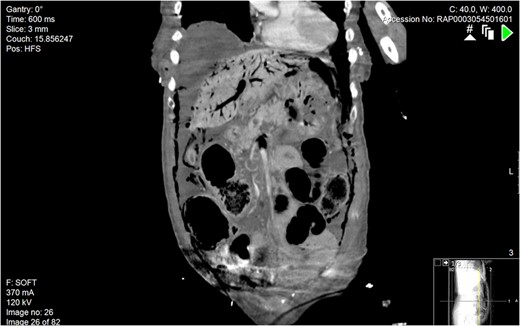
Coronal section of abdominal CT scan. A large amount of gas can be seen within the hepatic portal venous system.
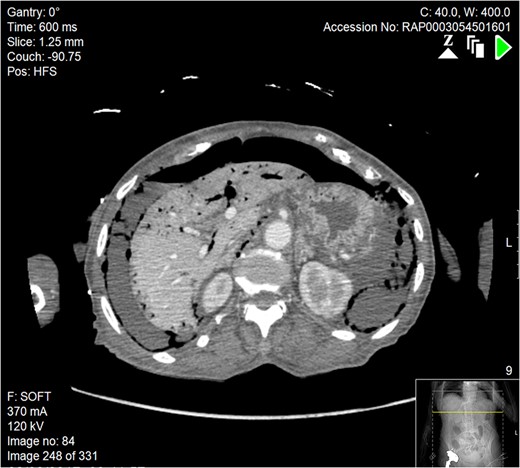
Axial section of abdominal CT scan. There is a significant quantity of free air and fluid within the abdomen, which can be seen adjacent to the liver, indicative of bowel perforation. Free air can also be seen in the portal venous system of the liver.
Due to the severity of the CT findings and calculation of peri-operative mortality risk, it was deemed that surgical intervention would not be of benefit. After discussion with the family the patient was treated palliatively. The patient died shortly afterwards, with the recorded cause of death being peritonitis, secondary to perforated ischaemic bowel. Significantly, the abdomen remained soft throughout the patient’s admission.
DISCUSSION
HPVG is a radiological sign first described by Wolfe and Evans in 1955 [1]. Nowadays, it is a recognized, but rarely identified complication of many acute gastrointestinal disorders including, colitis, ischaemia and perforation [2, 3, 4]. Signs and symptoms associated with the radiological finding of HPVG are varied, and little is understood of its pathogenesis, likely connected to gas forming organisms in the bowel lumen or portal venous system. A strong index of suspicion is required for prompt scanning and subsequent treatment of a potentially sinister underlying disease process [4, 5]. HPVG is a poor prognostic indicator with most cases ultimately proving terminal, often due to subsequent bowel necrosis [5, 6].
Bowel ischaemia is a known cause of HPVG. Furthermore, it is important to note that in this case the CTCAP did not highlight pneumatosis intestinalis (PI); HPVG with PI usually indicates intestinal ischaemia, and therefore increases urgency to operate. However, many causes of HPVG without PI are benign [6]. As the above case highlights, HPVG can be found in patients who on admission were remarkably well, with insidious onset of symptoms including constipation and abdominal pain. This presentation could have been secondary to constipation and venous stasis. As the appearance of HPVG is usually seen in the pre-morbid setting, clinical efforts should be focused on both the prevention and prompt management of the underlying cause such as bowel perforation, as treatment to avoid death is challenging. In cases where doubt exists, a laparoscopic exploratory procedure will be pivotal in excluding a surgically treatable disease [6].
CONFLICT OF INTEREST STATEMENT
None declared.
FUNDING
This work was partly supported by the Department of Surgery, North Middlesex Hospital.
REFERENCES
- abdominal pain
- computed tomography
- arterial blood gas
- constipation
- enema solution
- emergency service, hospital
- feces
- glasgow coma scale
- intestines
- lactates
- necrosis
- phosphates
- abdomen
- enema administration
- pelvis
- patient prognosis
- rectal examination
- abdominal examination
- air fluid level
- older adult
- effusion
- portal venous gas



