-
PDF
- Split View
-
Views
-
Cite
Cite
Laura Washburn, N Thao Galván, Sadhna Dhingra, Abbas Rana, John A Goss, Histoplasmosis hepatitis after orthotopic liver transplantation, Journal of Surgical Case Reports, Volume 2017, Issue 12, December 2017, rjx232, https://doi.org/10.1093/jscr/rjx232
Close - Share Icon Share
Abstract
Histoplasmosis is an endemic mycosis in the Ohio and Mississippi River valleys and can cause disseminated infection in immunocompromised hosts. Disseminated histoplasmosis is often respiratory in nature and most cases in transplant patients occur within 2 years post-transplantation. A 32-year-old male on mycophenolate and tacrolimus who underwent an orthotopic liver transplantation 10 years prior presented with generalized body aches, fevers, mild congestion, dysuria and elevated transaminases. Liver biopsy revealed epithelioid granulomas with narrow-based budding yeast, suggesting histoplasma. Liver involvement in disseminated histoplasmosis is well characterized however the disease is usually pulmonary in origin. Only three other case reports describe isolated granulomatous hepatitis, and this is the first to our knowledge to occur in a liver transplant allograft. A high index of suspicion is essential for diagnosis and prompt treatment of histoplasmosis in transplant patients considering their immunocompromised state.
INTRODUCTION
Histoplasmosis is the most common endemic mycosis in the USA as well as certain areas of Latin America and, of the endemic mycoses, is one of the most fatal. The increasing use of immunosuppressive medications, such as tumor necrosis factor and calcineurin inhibitors, has resulted in rising incidence of the fungal infection, which is particularly relevant to the transplant population [1]. It is intensely endemic to the Ohio and Mississippi River valleys, and found in bird and bat guano. Infection usually involves inhaling an inoculum of Histoplasmacapsulatum and with the inactivation of T lymphocytes by calcineurin inhibitors, macrophages are not initiated to inhibit the growth of the fungal infection, leading to increased fungal burden and mortality [2]. Here we describe a case of Histoplasmosis hepatitis in a liver transplant recipient 10 years out from his transplantation, with histopathology illustrating the yeast-like fungal elements.
CASE REPORT
The patient is a 32-year-old man who, in 2006, underwent an orthotopic liver transplantation for Glycogen Storage Disease Type 3. He had been doing well since transplant until 2012 when he was found to have slightly elevated transaminases (AST 156 U/L, reference range 5-34 U/L) (ALT 107, reference range 6-55 U/L) on mycophenolate and tacrolimus. Ultrasound imaging showed a normal liver transplant allograft with excellent perfusion. A percutaneous fine needle liver biopsy revealed no acute cellular rejection, but with nonspecific and minimal minute foci of necrosis and minimal lymphocytic cholangitis. Because he had aphthous ulcers, his mycophenolate was decreased. His mildly elevated transaminases persisted in a hepatocellular pattern through the years, up to the 200 s U/L. A subsequent biopsy in April 2015 was equally equivocal with minimal lobular spotty necrosis and bile ductular proliferation, yet no signs of rejection. In October 2016, another liver biopsy showed mild lobular inflammation with mild portal inflammation and focal mild bile duct damage. The progressive findings in the liver biopsies were described as minimal and nonspecific but a differential diagnosis included drug-induced liver injury, viral hepatitis, or acute cellular rejection. Because this could be an atypical pattern of acute cellular rejection, steroid therapy was added.
In March 2017, the patient presented with 2 weeks of generalized body aches, fevers, mild congestion and dysuria. His transaminases worsened—AST 360 U/L, ALT 387 U/L. Blood, urine and sputum cultures grew no organisms and the patient had a normal chest radiograph and abdominal ultrasound. CT sinus, obtained to rule out sinusitis, remarked on few mucous retention cysts of the maxillary sinuses, but was otherwise negative for any other pathology. However, further interrogation found that the patient had significant opportunistic infection exposure risk; the patient was a butcher at a local grocery store, and owned a new rabbit, several parakeets and four dogs. A repeat liver biopsy was performed, and this time, was found to have predominantly lobular, and occasionally portal, epithelioid granulomas (Fig. 1) with intracellular yeast-like elements (Fig. 2). These were described as narrow-based budding yeasts favoring histoplasma (Fig. 3). No portal based features of acute rejection were noted and bile ducts were preserved in the majority of portal tracts. Urine histoplasma antigen testing corroborated the histology finding—the patient had progressive disseminated histoplasmosis manifested as granulomatous hepatitis. He completed an 11-day course of liposomal amphotericin B and will continue itraconazole therapy for a year. His immunosuppression regimen was significantly decreased and mycophenolate was stopped. The most recent liver biopsy in May 2017 revealed a persistent—though significantly decreased—lobular inflammation, microgranulomas and budding yeast elements. His transaminases remain elevated at AST 265 U/L and ALT 259 U/L. He will continue close follow up to ensure further improvement on current therapy and resolution of Histoplasmosis.
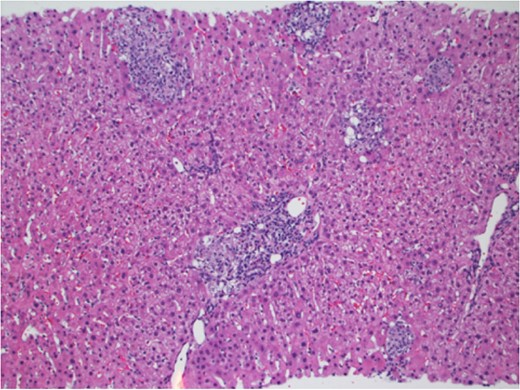
Liver parenchyma with multiple discrete portal and lobular granulomas. Hematoxylin and Eosin stain ×100.
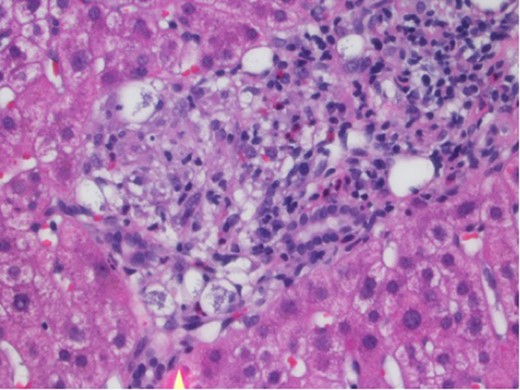
Portal granuloma with histiocytes containing multiple intracytoplasmic yeast-like fungi. Hematoxylin and Eosin stain ×400.

Grocott methanamine silver stain showing yeast-like fungi with narrow-based budding, consistent with histoplasma ×400.
DISCUSSION
Symptoms of Histoplasmosis are often respiratory in nature, as it is a predominantly confined to the lungs. However, once the pathogen disseminates extracellularly through blood or lymph, macrophages or neutrophils, it becomes a progressive disseminated histoplasmosis with symptoms that reflect diverse end organ effects, as in this case [3]. Histoplasmosis in transplant patients has been well described, often as an early diagnosis, with more than two-third of cases described within the first 2 years of transplantation [1]. This case, contracted 10 years later, serves as the first to our knowledge that illustrates granulomas and intracytoplasmic yeast-like fungi within the liver parenchyma of the transplant allograft. Furthermore, only three other reports are of isolated granulomatous hepatitis, and ours serves as the only one to report this finding in a liver transplant allograft [4–6]. Immunocompetent hosts can often develop antigen-specific CD4 T lymphocyte-mediated immune response which can limit the disease. However, H. capsulatum can establish a quiescent phase indefinitely, and so for the immunocompromised host, reactivation will continue to serve as a threat, as in this case [7]. Our patient will need to continue antifungal therapy, likely for a year, with surveillance of his antigenuria, which has been suggested to correlate with fungal burden [2].
CONFLICT OF INTEREST STATEMENT
None declared.
REFERENCES
- mycophenolate mofetil
- lung
- mycoses
- dysuria
- fever
- generalized body pains
- granulomatous hepatitis
- histoplasmosis
- hepatitis
- granuloma
- histoplasma
- immunocompromised host
- liver transplantation
- mississippi
- ohio
- saccharomycetales
- infections
- diagnosis
- liver
- tacrolimus
- transplantation
- liver biopsy
- liver transplant, orthotopic
- disseminated histoplasmosis
- allografting
- transaminitis



