-
PDF
- Split View
-
Views
-
Cite
Cite
M Wähmann, M Wähmann, F Schütz, C Sohn, S Schott, T Kremer, J F Hernekamp, U Kneser, Severe Fournier’s gangrene—a conjoint challenge of gynaecology and plastic surgery, Journal of Surgical Case Reports, Volume 2017, Issue 12, December 2017, rjx239, https://doi.org/10.1093/jscr/rjx239
Close - Share Icon Share
Abstract
Necrotizing fasciitis (NF) is a rare soft tissue infection characterized by rapidly progressing necroses and a high mortality. Prompt diagnosis and immediate medical treatment including radical debridement and broad spectrum antibiotics are the key to successful management. We report on a 46-year-old diabetic female who developed extensive, deep necroses in the perineal area and proximal thighs within a few days. After initial gynaecological consultation, she was transferred directly to our department. Due to the suspicion of NF, an immediate radical debridement was performed. Two more debridements were necessary to control the infection. After stabilization, the extensive soft tissue defect was reconstructed using a combination of plastic reconstructive procedures. Due to early diagnosis, direct referral and immediate surgical treatment, the patient survived.
INTRODUCTION
Necrotizing fasciitis (NF) is a rapid progressive soft tissue infection that is characterized initially by fascial necroses that may lead to alterations of subcutaneousadipose tissue and local skin [1]. The specific form manifesting in the genital and perineal regions was described as a so-called ‘Fournier gangrene’ [2]. With an incidence of 0.4–1/100 000 [1], this soft tissue infection is rare [3], but an increasing incidence can be observed in recent years [1, 4]. The most frequent comorbidities are diabetes mellitus, obesity, chronic renal insufficiency and immunosuppression [5]. Overall, the bacterial spectrum of NF patients is broad with over 75 detected pathogens [6].
Whereas, the port of entry for the bacteria is generally small, the infection reaches the fascial layer and rapidly progresses in the deep soft tissues. Consequently, superficial symptoms such as redness, skin hyperthermia and blister occur lately during the course of the disease. Since systemic inflammatory symptoms can develop fulminantly, immediate surgical interventions with radical debridement of infected soft tissues and the surrounding skin must be performed [7]. Non-specific signs of infection, such as erythema, local hyperthermia or fever may lead to possible differential diagnoses such as erysipelas, streptococcal myositis, gas gangrene or the streptococcal-induced toxic shock syndrome, thus making early diagnosis difficult. A misdiagnosis can lead to delayed surgical treatment, which results in a high fatality rate.
CASE REPORT
A 46-year-old female patient developed large-scale, map-like necroses of the mons pubis and the right inner thigh. The comorbidities of the patient were hypertension, obesity, type 2 diabetes mellitus and nicotine abuse. First, the patient was referred to a gynaecological university clinic and showed a systemic inflammatory response (leucocytosis: 12.8 × 103/μl; C-reactive protein: 183.5 mg/l), fever and a poor general condition. She was immediately transferred to our department for surgical treatment, because NF was suspected. At admission, the patient developed a septic shock as well as skin necroses, reddening and skin hyperthermia (Fig. 1). Since the patient’s symptoms rapidly progressed, she was immediately taken to the operation theatre and a radical necrosectomy of the affected areas was performed. The real extent of the disease was observed intraoperatively, since the area of lytic fascia, grey fluid (‘dishwater pus’) and infected soft tissues far exceeded the initially visible necrotic zones (Fig. 2a and b). Intraoperatively, fascial samples were taken for histological and microbiological examination as well as blood cultures. A calculated triple antibiotic treatment with penicillin, clindamycin and meronem was applied. Postoperatively, the patient required catecholamines and was admitted to the burn unit. Two more debridements were required until the infection was finally controlled. The microbiological evaluation of the tissue samples revealed a polymicrobial infection with detection of, among others, streptococci, various enterobacteria strains and anaerobic gram-positive germs in the blood cultures. In the histopathological analysis, the suspect diagnosis of an NF was confirmed. Necrotic fibrous, connective tissue with granulocytic infiltrations and a septic thrombovasculitis were observed.

Fluctuating erythema, blisters and necrotic areas at admission of the patient.
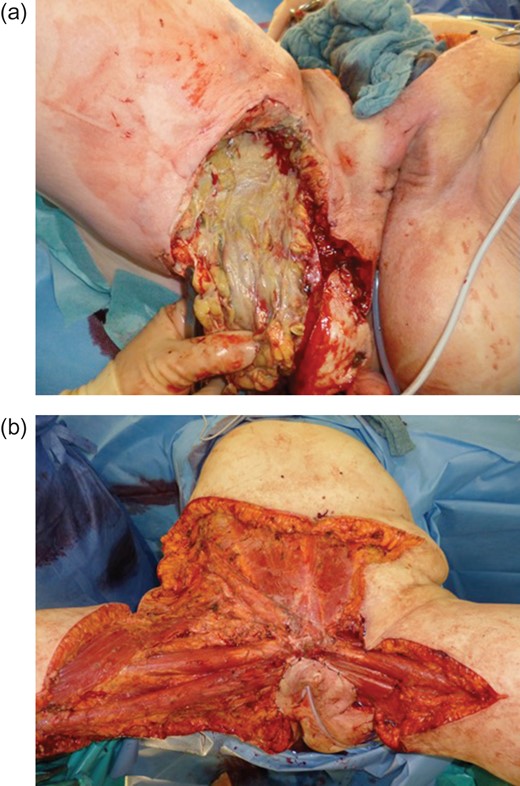
(a) Lytic-necrotic fascias and the subcutaneous soft tissue intraoperatively. (b) Clinical appearance after radical debridement of the infected areas on the first day.
After a stabilization period of frequent dressing changes and open wound therapy, a two-stage reconstructive approach could be planned. During the first procedure, the femoral vessels, which were exposed on both sides, were covered by two pedicled sartorius flaps. Additionally, the open wound area was reduced using split thickness skin grafting. However, the os pubis and the symphysis remained exposed. Here, a pedicled fasciocutaneous anteromedial thigh (AMT) perforator flap was applied for reconstruction. The flap was pulled under the sartorius muscle and was inserted into the defect.
Five months postoperatively, the results were functionally satisfying (Fig. 3a and b). However, further reconstructive procedures were performed after 11 months to resolve a painful scar cranial to the clitoris and to reconstruct the external genitalia. An interdisciplinary plastic reconstruction was performed including gynaecologists and plastic surgeons. Here, a perforator-based flap from the left thigh/buttocks as well as an advancement of the AMT flap were performed (Fig. 4a and b). In the final clinical check-up 4 months later, the patient reported having recovered a sufficiently good quality of life, especially the ability for cohabitation (Fig. 5).
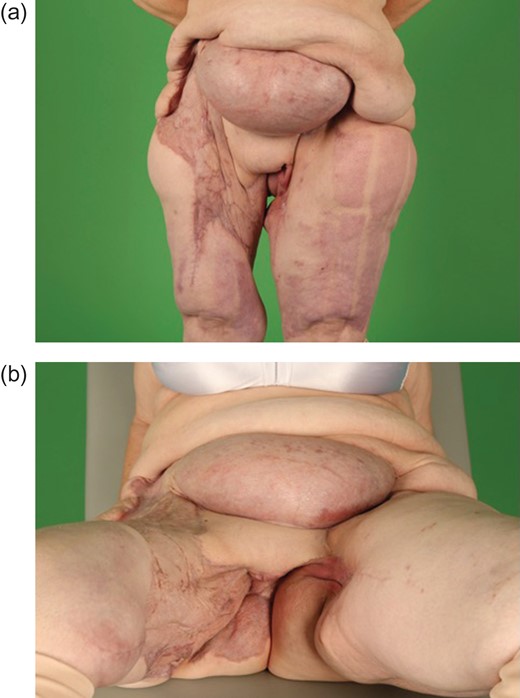
(a) and (b) Stable reconstructive result 5 months postoperatively.
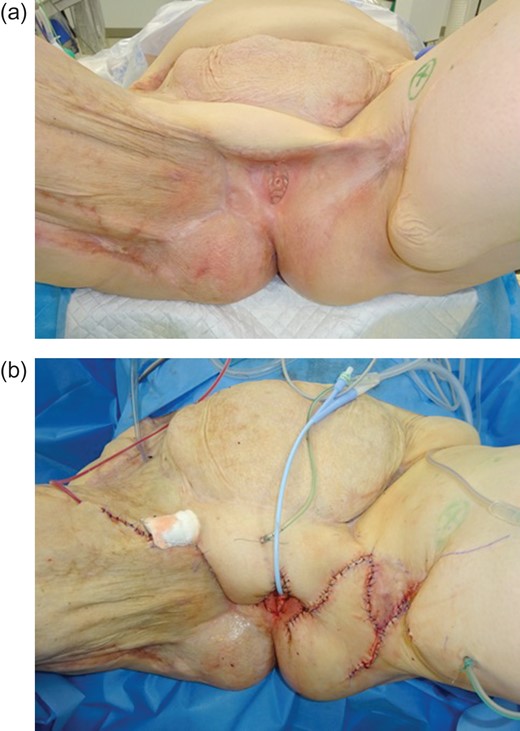
(a) Preoperative findings with clearly visible transverse scars and missing external genitalia (11 months after initial diagnosis). (b) Release of consecutive scarring and plastic reconstruction of the external genitalia.

Postoperative result 5 months after last reconstructive procedure.
DISCUSSION
The described patient case is exemplary of the typical picture of a NF of the perigenital region with fulminant course.
The aetiology of this severe soft tissue infection has to date not been sufficiently clarified. Diagnostics focus on clinical symptoms. In addition to the initially rather non-specific signs of inflammation, a marked pain (‘pain out of proportion’) is the dominant symptom in the early stages, caused by the spread of fascial ischaemia [8]. In the emergency room, the patients’ symptoms with reduced mental condition and cardiocirculatory depression already suggested septicaemia. In the presented case, preoperative radiological diagnostics were not performed to avoid time loss. In the authors opinion, radiologic examinations such as magnetic resonance tomography or computed tomography should be reserved for rare cases, since time is critical and diagnosis can be performed clinically. Therefore, surgical intervention simultaneously allows diagnosis as well as treatment. The fastest possible radical debridement of the infected and necrotic soft tissues has the highest priority during the acute therapy. Intraoperatively, an uncompromised debridement (‘be bloody, bold and resolute’) is mandatory [9] and patients might even require mass transfusion and advanced coagulation management. Typical intraoperative clinical signs are a greyish-necrotic fascia as well as milky cloudy fluid (‘dishwater pus’). In addition to the surgical debridement, a broad intravenous triple antibiotic treatment (penicillins, lincosamides and carbonpenems) is indicated. Due to the mostly complex surface therapy and intensive medical care, an early transfer to a centre with a burn- or critical wound care unit is reasonable, whereby the fatality rate can be reduced to ~20% [10].
In most cases, several debridements are necessary to radically remove the infected soft tissues before attempting soft tissue reconstruction. In our case, a bilateral sartorius flap was vital because of the risk of vascular erosion of the exposed femoral vessels. Stable wound closure and function has a higher priority than the aesthetic result (‘form follows function’). However, the patient survived and has a satisfying quality of life, although an NF localized on the trunk includes higher mortality rates than other localizations such as the extremities [7].
CONFLICT OF INTEREST STATEMENT
We declare that we have no conflict of interests. The clinical data have been evaluated exclusively in our department. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
REFERENCES
- antibiotics
- diabetes mellitus
- patient referral
- consultation
- debridement
- necrotizing fasciitis
- fournier gangrene
- gynecology
- necrosis
- anogenital region
- soft tissue infections
- surgical procedures, operative
- thigh
- infections
- diagnosis
- mortality
- stabilization
- early diagnosis
- soft tissue
- medical management



