-
PDF
- Split View
-
Views
-
Cite
Cite
Joel Hardman, Christopher Toon, Arjuna Nirmalananda, An unusual presentation of eosinophilic angiocentric fibrosis, Journal of Surgical Case Reports, Volume 2017, Issue 12, December 2017, rjx234, https://doi.org/10.1093/jscr/rjx234
Close - Share Icon Share
Abstract
Eosinophilic angiocentric fibrosis (EAF) is a rare, benign condition affecting the respiratory mucosa and is generally characterized by a locally destructive growth. We present a case of a lady with a saddle nose deformity that had for many years been treated as granulomatosis with polyangiitis (GPA), of which saddle nose deformity is a classic feature. At the time of surgery, she was found to have subglottic stenosis another classic feature of GPA, however, histology demonstrated EAF. We discuss the difference between the two conditions and highlight the importance of making the correct diagnosis.
INTRODUCTION
Eosinophilic angiocentric fibrosis (EAF) is a rare, benign condition affecting the nasal cavity and paranasal sinuses, lacrimal glands and lower respiratory tract. It is slowly progressive and usually presents clinically as a locally destructive growth with nasal obstruction, epistaxis or deformity [1]. The characteristic histological appearance includes a perivascular eosinophilic-rich inflammatory infiltrate with concentric fibrosis [2]. It is now generally included as a subset of IgG4-related disorders [3].
Our understanding of inflammatory disorders is evolving with the clinical and pathological features still being defined and the overlap between conditions being clarified. This case demonstrates a clinical similarity between granulomatosis with polyangiitis (GPA) and EAF.
CASE REPORT
A 62-year-old female was referred to ear, nose and throat services for assessment and management of nasal obstruction. She had previously been treated for GPA. It was a presumptive diagnosis as the nasal tissue biopsies, taken during a septoplasty several years previously, had been misplaced and tissue confirmation of the condition had never been made. She was treated with various courses of immune modulating drugs and corticosteroids. However after a subsequent second Rheumatology opinion, it was felt GPA was unlikely and she was weaned off these medications. Her anti-neutrophil cytoplasmic antibody (ANCA) levels had always been negative and IgG4 levels were normal.
The patient also had diabetes and obstructive sleep apnoea for which she used continuous positive airway pressure (CPAP) machine. Over the preceding 10 years, she had a number of episodes of exertional shortness of breath and with the diagnosis of GPA, there was a concern of subglottic stenosis, though this had never been definitively demonstrated.
After review by a rhinologist (senior author, A.N.), her nasal obstruction was attributed to her significant saddle deformity of the mid portion of the nose (Fig. 1). There was also thickening of the right septal mucosa, assumed to be secondary to the previous surgery. Given the functional effect of the deformity as well as the cosmetic concerns she had, surgery was offered.

Clinical photographs demonstrating saddle nose deformity with collapse of the nasal dorsum (A) anterior view and (B) lateral view.
As there was speculation of subglottic stenosis in the context of presumed GPA, it was felt that an airway assessment was required prior to elective surgery. Flexible nasendoscopy was performed in the operating theatre demonstrating moderate subglottic stenosis. General anaesthesia was commenced though it was not possible to pass a 4-mm microlaryngoscopy endotracheal tube due to the stenosis. She was sufficiently maintained on a laryngeal mask airway and the operation progressed as planned.
Surgery included inferior turbinate reduction and external rhinoseptoplasty with conchal cartilage graft. The septal mucosal thickening was excised as part of the surgery and sent for histopathology. The conchal cartilage was used to reconstruct the saddle deformity. The surgery proceeded uneventfully.
Histopathology demonstrated stromal storiform and perivascular concentric fibrosis with a prominent chronic inflammatory infiltrate (Fig. 2). This consisted of mature lymphocytes, mature plasma cells and eosinophils (Fig. 3). Arteritis (a feature of GPA) was not seen. On digital microscopy, the IgG4 plasma cell counts were 98–120/HPF and IgG4:IgG ratios of 0.4–0.7.
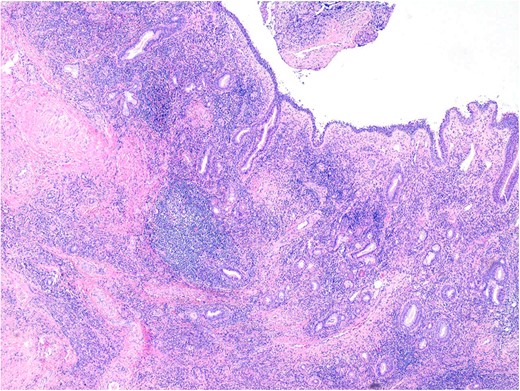
Sinonasal mucosa showing marked chronic inflammation and stromal fibrosis. 40× magnification. H&E.
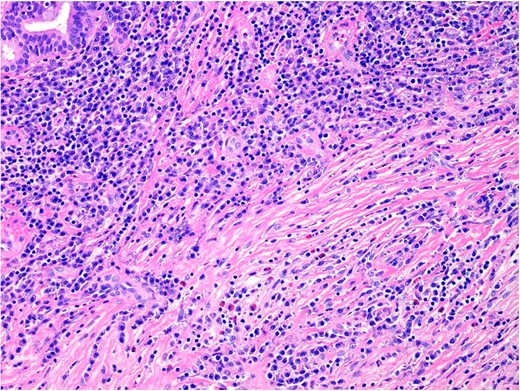
The inflammatory infiltrate is composed of mature lymphocytes, plasma cells and eosinophils. 200× magnification. H&E.
At 3 months following surgery, the patient had significant improvement in her nasal obstruction and was satisfied with the cosmetic changes. She remains systemically well.
DISCUSSION
EAF is an uncommon cause of nasal obstruction. The most common presentation is a sinonasal mass or mucosal thickening. Nasal deformity is seen as a result of cartilage destruction. The clinical combination of saddle nasal deformity and subglottic stenosis is classically associated with GPA. Fageeh et al. [4] described a case of EAF involving the larynx and Deshpande et al. [5] reported that EAF can involve the lower airway. Loane et al. [6] reported a case in which a patient with ANCA positive multi-system GPA developed nasal obstruction and was subsequently shown to also have EAF. Kobraei et al. [7] described the case of women with a recurrent lower tracheal mass that was subsequently proven to be EAF.
It is important to distinguish between the conditions as GPA is a systemic condition potentially affecting multiple organs and the mainstay of treatments are glucocorticoids as well as immune modulating therapies such as mycophenolate and methotrexate [8]. Both these drugs are good at controlling inflammation but can have significant side effects. In comparison, EAF is a disease of the airway and surgery alone has generally been the main treatment.
IgG4-related diseases are a collection of inflammatory conditions that affect a variety of organs in the body, including the pancreas, lungs, kidneys and salivary glands. Serum IgG4 is only elevated in 50% of patients. The diagnosis is generally made on histology. Elevated IgG4-related plasma cells and an IgG4:IgG ratio >0.4 support the diagnosis [3].
In a recent systematic review article, 52 cases of EAF were identified from the literature [1]. We have presented a case that demonstrates a rare feature, namely subglottic stenosis. We have also highlighted the importance of accurate tissue diagnosis to ensure the correct diagnosis is made, allowing the appropriate treatment.
CONFLICT OF INTEREST STATEMENT
None declared.
FUNDING
There was no external support or conflict of interest in the preparation of this manuscript, which has not been submitted or published elsewhere.



