-
PDF
- Split View
-
Views
-
Cite
Cite
Ioannis D Kostakis, Zoe Garoufalia, Themistoklis Feretis, Stylianos Kykalos, Dimitrios Mantas, A case of Bouveret’s syndrome treated with gastrojejunal anastomosis, Journal of Surgical Case Reports, Volume 2017, Issue 10, October 2017, rjx213, https://doi.org/10.1093/jscr/rjx213
Close - Share Icon Share
Abstract
Bouveret’s syndrome is a rare cause of proximal gallstone ileus with obstruction of duodenum or gastric outlet. We report a case of an 87-year-old female patient presented with 1 week history of vomiting whose plain radiograms showed ileus and pneumobilia. The abdominal computed tomography confirmed pneumobilia and revealed free air and leakage of oral contrast agent in the hepatic hilum and subhepatic space and an impacted gallstone in the third portion of the duodenum. The patient underwent exploratory laparotomy, which showed that the duodenal perforation was circumvallated, and a side-to-side retrocolic gastrojejunal anastomosis was performed in order to surpass the impacted gallstone. Removal of the impacted gallstone through enterotomy or gastrotomy or endoscopic lithotripsy is the usual treatment of Bouveret’s syndrome. However, gastrojejunal bypass may be a treatment option when the patient undergoes laparotomy and the gallstone is impacted in the third or fourth portion of the duodenum.
INTRODUCTION
Gallstone ileus is a rare cause of intestinal obstruction, comprising 1–4% of cases of obstructive ileus [1, 2]. It is caused by the migration and impaction of gallstones to intestines through a cholecystoenteric fistula, which is caused due to erosion of gallbladder and intestinal wall by the gallstones [1–3]. Obstruction of duodenal lumen or gastric outlet from a large gallstone that has migrated to the duodenum through a cholecysto-duodenal fistula is a rare form of gallstone ileus, which is characterized as Bouveret’s syndrome [1–4]. Herein, we present a case of Bouveret’s syndrome that was treated with gastrojejunal anastomosis.
CASE REPORT
An 87-year-female patient was admitted to emergency department complaining about vomiting for the past 7 days with mild abdominal pain. The patient was hemodynamically stable, had sluggish bowel sounds and soft abdominal wall with mild tenderness. The patient also suffered from atrial fibrillation, heart failure, myelodysplastic syndrome, hiatus hernia and cholelithiasis. The findings of the laboratory tests were unremarkable. Plain chest and abdominal radiograms revealed hiatus hernia with gastric dilation (Fig. 1), a few air-fluid levels and pneumobilia, with delineation of extrahepatic and intrahepatic bile ducts by air (Fig. 2). A nasogastric tube was inserted, which drained biliary content. An abdominal computed tomography (CT) scan revealed the presence of air in the intrahepatic bile ducts, free air and leakage of oral contrast agent in the hepatic hilum and subhepatic space and an impacted gallstone in the third portion of the duodenum (Figs 3 and 4). The diagnosis of cholecystoenteric fistula and proximal gallstone ileus was set.
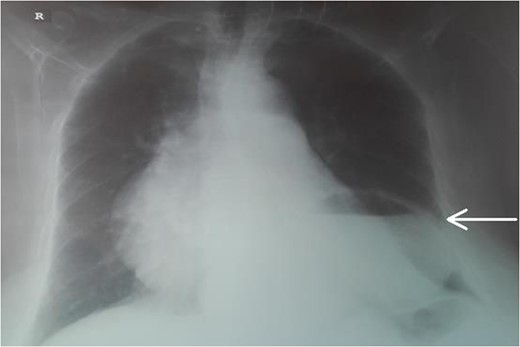
Chest radiogram. The arrow shows the dilated intrathoracic stomach.
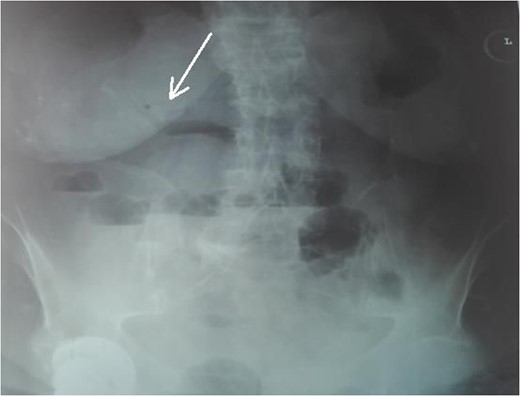
Abdominal radiogram. The arrow shows the air in the bile ducts.
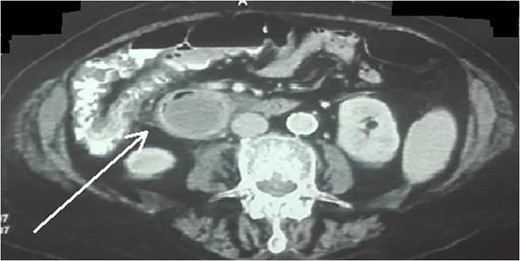
Abdominal CT scan (axial plane). The arrow shows the impacted gallstone.
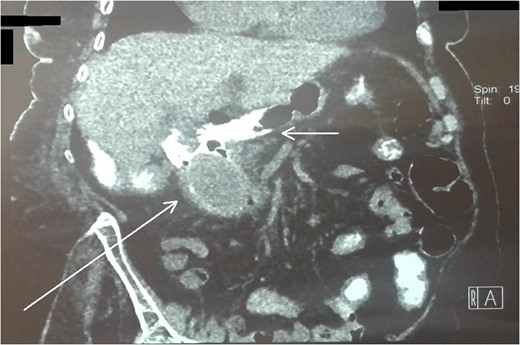
Abdominal CT scan (coronal plane). The long arrow shows the impacted gallstone and the short arrow shows the free air and the leakage of oral contrast agent.
The patient underwent exploratory laparotomy the same day, which revealed gallbladder, duodenum, liver edge and right colic flexure to be covered by greater omentum and a hard lump with regular contour within the third portion of the duodenum. A side-to-side retrocolic gastrojejunal anastomosis was performed at 30 cm from the ligament of Treitz using staplers. After an initially uneventful postoperative course, hematemesis and hemodynamic instability were observed on the 9th day. After hemodynamic stabilization with crystalloids, colloids and blood transfusion, the patient underwent an esophagogastroduodenoscopy, which showed an adherent clot on the anastomosis without active bleeding and the impacted gallstone in the third portion of the duodenum. Thus, hematemesis was attributed to a transient hemorrhage from the anastomotic site of gastrojejunostomy. The patient was treated conservatively with administration of blood and fresh frozen plasma and temporary interruption of the prophylactic low molecular weight heparin. Oral nutrition was gradually reinstituted from the 13th postoperative day on, and the patient was discharged on the 26th postoperative day in good condition.
DISCUSSION
As it was mentioned previously, Bouveret’s syndrome is a rare form of gallstone ileus [1–4]. Clinical symptoms are non-specific and it is most commonly presented with nausea, vomiting, early satiety and abdominal pain [1, 3]. The typical radiological findings comprise Rigler’s triad [presence of small-bowel obstruction and dilated stomach, pneumobilia (air in the biliary tree) and ectopic gallstones], which can be detected in plain abdominal radiograms or abdominal CT scan, but it is not always present. CT scan may also demonstrate the presence of cholecysto-duodenal fistula by administrating oral or air contrast material [1–3]. Removal of the impacted gallstone through enterotomy or gastrotomy or endoscopic lithotripsy is the usual treatment. In particular, the non-surgical treatment options include endoscopic mechanical, electrohydraulic or laser lithotripsy and extracorporeal shockwave lithotripsy, either alone or combined. However, there is the possibility of distal migration of fragments, which may cause distal ileus and eventually require surgical removal [1, 3, 4]. In our case, the free air and leakage of oral contrast agent in the abdominal CT scan pointed out the need for exploratory laparotomy. The fact that the site of perforation was circumvallated and the difficult accessibility of the third portion of the duodenum led us to perform a gastrojejunal bypass in order to surpass the impacted gallstone. Another reason why we selected this atypical management was the advanced age and multiple comorbidities of the patient, which prevented us from trying to repair the cholecysto-duodenal fistula or remove the impacted gallstone, and instead led us to adopt a minor and shorter operation. In conclusion, gastrojejunal bypass may be a treatment option when the patient undergoes laparotomy and the gallstone is impacted in the third or fourth portion of the duodenum.
CONFLICT OF INTEREST STATEMENT
No conflicts of interest.
FUNDING
No funding.



