-
PDF
- Split View
-
Views
-
Cite
Cite
Ruiping Zhang, Jungang Liu, Yizheng Wang, Lirong Cao, Chunquan Cai, Sub-capsular effusion of liver as a rare complication of ventriculoperitoneal shunt in a child, Journal of Surgical Case Reports, Volume 2017, Issue 10, October 2017, rjx211, https://doi.org/10.1093/jscr/rjx211
Close - Share Icon Share
Abstract
The most common procedure to deal with hydrocephalus is ventriculoperitoneal (VP) shunt. The purpose of the shunt is to drain cerebrospinal fluid from cerebral ventricles to abdominal cavity. Many complications of VP shunts have been reported such as infection, obstruction, overdrainage. Abdominal complications occur in ~15–25% of VP shunts in pediatric patients, such as peritonitis, hernia, abscess, perforated colon, perforated bladder and abdominal pseudocyst. However, sub-capsular effusion of liver is a rare complication of VP shunt. In this case report, We described an unusual case of VP shunt complication in a 2-year-old child who presented with intermittent fever and abdominal pain.
INTRODUCTION
Ventriculoperitoneal (VP) shunt is one of the most frequent treatment for hydrocephalus [1], used to drained excessive cerebrospinal fluid (CSF) accumulated in cerebral ventricles into abdominal cavity to balance the secretion and absorption of CSF. However, the incidence of complications of VP shunt was up to 30% [2, 3]. Abdominal complications occurred in ~15–25% of VP shunts, such as peritonitis, hernia, abscess, perforated colon, perforated bladder and abdominal pseudocyst [4]. In this case report and literature review, we discussed a rare case of sub-capsular effusion of liver after VP shunt, and also discussed management method to deal with it.
CASE REPORT
A female child, at the age of 2 years, was admitted to our hospital because she was not able to walk alone. This child patient had undergone ventriculo–peritoneal (VP) shunt procedure for hydrocephalus confirmed by magnetic resonance imaging (MRI). On the 50th day after the surgery, she mainly complained of intermittent fever and mild abdominal pain for 12 days. Physical examination showed no obvious abnormality. Blood routine examination showed white blood cell count was 8.31 × 109/l, with neutrophils 60.7%, lymphocytes 30.8%. C-reactive protein was 81 mg/l. Abdominal ultrasonography indicated ascites. Abdominal enhanced computed tomography (CT) scan showed that water-like hypointense mass in sub-capsular of liver, which was homogeneous and well-defined, the max cross-sectional area was ~6.04 × 3.85 cm, multiple catheter images were seen in abdominal cavity, also showed that there was no enhanced images in the mass (Fig. 1). Accordingly, it was necessary to perform exploratory operation. Operation found that a little of clear fluid was accumulated in abdominal cavity and the distal end of catheter was located at the sub-capsular of diaphragmatic surface of right liver. The distal end was pulled out slowly and sub-capsular effusion overflowed. The VP shunt catheter was neither disconnected nor fractured, and was replaced subsequently in abdominal cavity. Postoperative CT scan showed that a small part of effusion remained in the liver contour and the distal catheter in the left abdominal cavity (Fig. 2). The child was discharged uneventfully in 1 week postoperative.
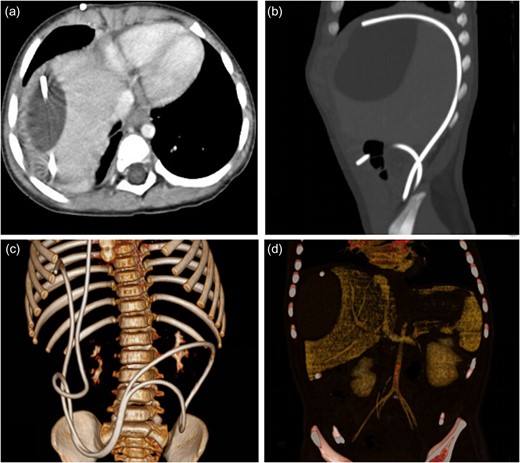
The enhanced CT before operation. (a) Axial CT showed water-like hypointense mass and catheter image in the liver contour. (b) Sagittal CT revealed catheter image under liver capsule and the homogeneous and well-defined mass in the liver contour. (c) Three-dimensional image of catheter in abdominal cavity. (d) The mass in the liver contour.
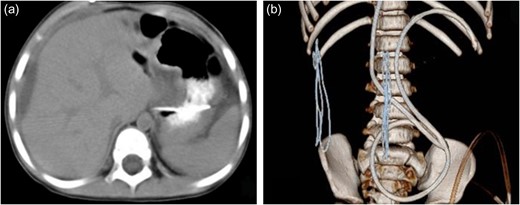
The CT scan after operation. (a) Axial CT revealed a small part of effusion remained in the liver contour. (b) Three-dimensional image of catheter showed the distal catheter in the left abdominal cavity.
DISCUSSION
VP shunt is the most common treatment for hydrocephalus. VP shunt plays an important role in managing hydrocephalus and has good efficiency on treatment options, but has the potential serious postoperative complications [1, 2]. Improper management might lead to shunt failure. According to the literature reported, the rate of complications of VP shunt was up to 30% [2, 3]. Common VP shunt complications included infections, obstruction and overdrainage [5]. In addition, complications occurred more frequently in children than in adults [6]. Abdominal complications occur in ~15–25% of VP shunts in pediatric patients [4], such as peritonitis, hernia, abscess, perforated colon, perforated bladder, perforated intestines and abdominal pseudocyst [4, 7, 8]. However, there is an unusual report of sub-capsular effusion of liver.
Abdominal complications occurred in liver is severe and rare, problem reported previously included liver abscess and liver pseudocyst [8, 9]. The main symptoms of them were fever, mild abdominal pain, similar to the presentation in our patient; the etiology was CSF from infected shunt into the abdomen, and intra-abdominal infection or biliary tract infection [8]. However, in present case, the reason of this complication was different from liver abscess and liver pseudocyst, it was due to operation failure, over-long catheter inserting into sub-capsular cavity of liver rather than liver parenchyma; therefore, liver injury was not obvious. Furthermore, the use of hard-tipped and sharp peritoneal catheters increased the risk of this complication [6]. Abdominal ultrasonography was an efficiency method to help diagnose. But in this case, abdominal ultrasonography showed normal other than ascites. Considering the history of VP shunt and the outcome of ultrasonography, it was necessary to carry out CT scan. In order to prevent this complication, laparoscopic abdominal insertion was worth applying in CSF shunt revision[10].
Here, we present a rare case of sub-capsular effusion of liver to improve the knowledge of VP shunt complications. We are aware of careful operation to avoid the occurrence of complications related to VP shunt. Furthermore, laparoscopic abdominal insertion is very important to reduce this complications [10]. Additionally, regular postoperative follow-up is most important to monitor possible complications. The prevention is always the best treatment.
ACKNOWLEDGEMENT
The authors thank the patient and her parents for allowing us to publish this case report.
CONFLICT OF INTEREST STATEMENT
The authors state that there is no conflict of interest.
FUNDING
This work was supported in part by grant 81771589 from the National Natural Science Foundation of China and grant 16KG166 from the Key Project of Tianjin Health Care Professionals and grant 2015KR12 from the Science and Technology Foundation of the Tianjin Bureau of Public Health.
REFERENCES
Author notes
These authors contributed equally to this work.



