-
PDF
- Split View
-
Views
-
Cite
Cite
Alessandro Tamburrini, Aurelio Majorino, Simon Duggan, Sanjay Jogai, Aiman Alzetani, A record-breaking lung metastasis from renal cell carcinoma 37 years after nephrectomy, Journal of Surgical Case Reports, Volume 2017, Issue 10, October 2017, rjx205, https://doi.org/10.1093/jscr/rjx205
Close - Share Icon Share
Abstract
Development of distant metastases from renal cell carcinoma (RCC) is a frequent occurrence and, in nearly 95% of the cases, secondary lesions present within 5 years following nephrectomy. We performed a left pneumonectomy for a peri-hilar lung mass in an 81-year-old man with history of kidney cancer, resected 37 years earlier. Histopathological examination revealed a solitary lung metastasis from RCC, relapsed after an extraordinary 37-year time interval. To the best of our knowledge, this remarkable case represents the longest time interval between radical nephrectomy for RCC and the occurrence of a pulmonary metastasis. After an uneventful post-operative recovery, there are no signs of disease recurrence at a 3-year follow-up. The possibility of a lung metastasis should be taken into account in patients with history of RCC who present with pulmonary nodules, even decades after treatment of the primary neoplasm.
INTRODUCTION
Renal cell carcinoma (RCC) is the most common renal malignancy and it accounts for ~2% of all the new diagnosis of cancer [1]. After radical nephrectomy, distant metastases are a frequent occurrence, presenting in up to 50% of the cases, with lungs being the most common target of secondary lesions [1]. Despite late recurrence of metastatic RCC has been previously reported [2–5], the greatest risk of recurrence is instead within the first 5 years following nephrectomy, with incidence as high as 93% [6]. We herein report an extraordinary case of a solitary lung metastasis from RCC presented 37 years after surgical resection of the primary tumour. To the best of our knowledge, this time interval is the longest ever between radical nephrectomy and pulmonary metastasectomy for RCC in the entire literature. We therefore consider it worth of report.
CASE REPORT
An 81-year-old man presented with a 2-month history of persistent cough and an abnormal chest x-ray showing a left upper lobe opacity. He was an ex-smoker and his past medical history was significant for hypertension, type 2 diabetes mellitus, and kidney cancer treated by radical nephrectomy 37 years earlier. Evaluation with [18F]-fluorodeoxyglucose-positron emission tomography/computed tomography revealed a large hypermetabolic peri-hilar left upper lobe lung neoplasm, in close proximity with the left main pulmonary artery (Fig. 1). No other lesions were detected elsewhere. Bronchoscopic citology brush was consistent for non–small-cell lung cancer and neoplastic involvement of mediastinal nodes was ruled out with endobronchial ultrasound. Global spirometry with transfer factor for carbon monoxide, echocardiogram and laboratory tests results were unremarkable. The patient was therefore deemed suitable for surgical resection. A left pneumonectomy and mediastinal nodal dissection was thus performed via a standard postero-lateral thoracotomy. Recovery after the operation was uneventful and the patient was discharged on post-operative Day 5. The histopathology findings were however significantly surprising. The tumour cells presented in solid islands and sheets, with distinct cytoplasmatic membranes, mild to moderately pleomorphic nuclei often with ‘raisinoid’ appearance and occasional binucleate cells. The cytoplasm was abundant and largely clear (Fig. 2). In view of the striking cytoplasmatic clearing, immunohistochemistry was also performed. The tumour cells were negative for CK5/6, p63, TTF-1, CD10, while there was a strong positivity for CK7 (Fig. 3) and CD117 (Fig. 4). The final diagnosis was therefore metastatic RCC, which had relapsed after the remarkably long period of 37 years, which is, to the best of our knowledge, the longest ever reported interval between surgery for RCC and the occurrence of a pulmonary metastasis. At 3-year follow-up, the patient is well and no recurrence of disease has been observed.
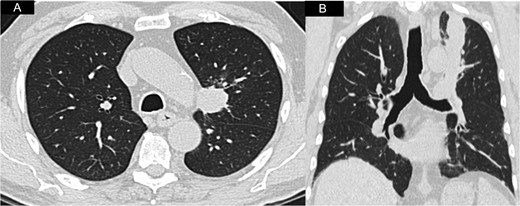
A and B Axial and coronal CT-scan view showing the left peri-hilar lung mass in close proximity to the main pulmonary artery.
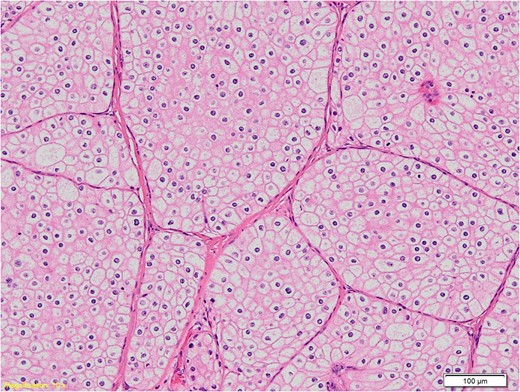
Histological section of the specimen, magnification 10×, hematoxylin-eosin staining: the tumour cells have well defined cell membranes and abundant cytoplasm that is pale eosinophilic to clear.
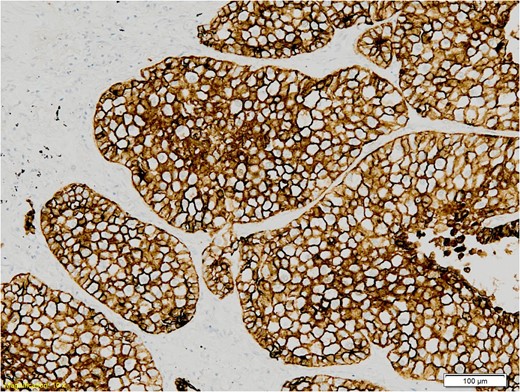
Himmunohistochemistry section of the specimen, magnification 10×: The tumour cells show strong membrane staining with CK7.
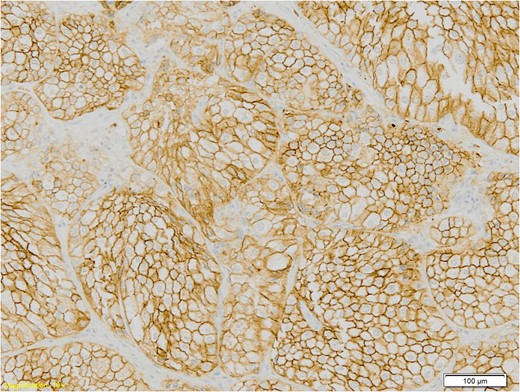
Himmunohistochemistry section of the specimen, magnification 10×: The tumour cells show strong membrane staining with CD117.
DISCUSSION
Development of distant metastases is a very common feature in the natural progression of RCC. Indeed, ~50–60% of the patients will present eventually metastatic disease requiring individual treatment decision [7]. The median time for tumour relapse following nephrectomy is 15–18 months, with 85% of recurrences occurring within the first 3 years [5] and 93% within the first 5 years [6]. Nevertheless, few remarkable cases of late metastatic presentation have been described [2–5]. Shiono et al. [2] reported a case of repeated lung metastasectomy 16, 24 and 25 years after treatment of RCC. In this patient, yearly follow-up scans were performed after the first metastasectomy, showing slow but progressive growth of initially millimetric lung nodules. All the resected lesions were metastases from clear cell type RCC. The same author [2] portrayed a mini review of the scant available literature, encompassing 25 years (1973–1998), where they described another five cases of late presentation of lung metastases from RCC, diagnosed between 20 and 28 years after resection of the primary neoplasm, with survival up to 4 years after metastasectomy. Watanabe and colleagues [5] recently reported the first case of pulmonary metastasectomy for RCC after an interval of over 30 years since nephrectomy. Their patient was an 82-year-old man in which a large solitary lung metastasis from RCC occurred 31 years after surgical treatment for primary tumour. A left upper lobectomy was performed in this case, and the patient was alive and disease-free at a 9 months follow-up. In our case instead, the lung metastasis occurred after an extraordinary 37 years interval after resection of RCC, therefore 6 years later than the above mentioned case [5]. In addition, our patient presented with a centrally located hilar mass, and we had to perform a left pneumonectomy which is still regarded as an operation with high morbidity risk. At the time of surgery, we suspected a primary lung cancer, rather than a secondary lesion. However, even for a metastasis, pneumonectomy would have been the surgical treatment of choice to achieve complete resection of all metastatic tissue, which is unanimously advocated as one of the mainstay principle in the surgical treatment of lung metastases [8]. In respect of RCC specifically, complete resection (R0) of all metastases has been also demonstrated to be an independent prognostic factor for patients’ survival after pulmonary metastasectomy [7, 9]. The other well-known prognostic indicators are the low number of metastases and a long disease-free interval (DFI) between the primary tumour and the development of lung lesions [7, 9]. Although it is generally accepted that a long DFI can be defined as a 3-year time [9], the definition of ‘long’ might be questionable when considering such an extraordinary case. The mechanisms behind these extremely delayed presentations of RCC metastases are obviously complex and far from being fully elucidated. The host’s immune mechanism has been hypothesized to play an important role in this setting, regulating and influencing tumour growth [10]. Normally, RCC is slow growing in nature, and such slow growth of initially microscopic metastases might receive an acceleration when the host’s immune competency is compromised [3]. A case described by Cozar et al. [4], where multiple late pulmonary metastases from a RCC treated 8 years earlier, developed only 2 months after an immunosuppressive treatment following renal transplant might give credit to this hypothesis. In conclusion, to the best of our knowledge this is so far the longest time interval between nephrectomy and lung metastasectomy for RCC (37 years). Pulmonary metastases from RCC can present even after a remarkably long period of time following treatment of primary cancer, perhaps due to a transient host’s immunosuppression which could upregulate tumour growth. In the evaluation of lung nodules of patients with history of RCC, the possibility of metastatic lesions should be considered even decades after nephrectomy.
CONFLICT OF INTEREST STATEMENT
The authors declare that there are no conflicts of interest regarding the publication of this paper.



