-
PDF
- Split View
-
Views
-
Cite
Cite
Alexandra W Elias, Dorin T Colibaseanu, Kristopher P Croome, Metachronous metastatic colonic small cell carcinoma and recurrent adenocarcinoma in a patient with ulcerative colitis, Journal of Surgical Case Reports, Volume 2017, Issue 10, October 2017, rjx201, https://doi.org/10.1093/jscr/rjx201
Close - Share Icon Share
Abstract
Colonic small cell carcinomas (SCCs) are rare, aggressive tumors characterized by early metastasis and poor prognosis. We describe a 39-year-old man with a history of ulcerative colitis and left colon adenocarcinoma resected at an outside institution who presented with hematochezia and proctalgia. Work-up revealed left colon SCC with liver metastases. After his excellent response to neoadjuvant chemotherapy, we performed synchronous proctocolectomy and right hepatectomy. Final pathologic evaluation revealed colonic primary SCC and recurrent adenocarcinoma with metastatic SCC to the liver; lymph nodes were positive for metastatic SCC and adenocarcinoma. SCC recurrence ultimately developed in the liver. To the best of our knowledge, this is the second reported case of surgical management of SCC of the colon with liver metastasis and the first report of synchronous excision. Despite superb response to neoadjuvant therapy and young patient age, caution is needed in surgical resection for SCC of the colon given the high recurrence risk.
INTRODUCTION
Colonic small cell carcinomas (SCCs) are rare, aggressive tumors with early metastasis and poor prognosis [1]. Approximately 100 reports have been published on SCC [2]. Its incidence comprises 0.1% of colorectal cancers [3, 4]. In cases of inflammatory bowel disease, the standardized incidence ratio of SCC is 1.7 [5]. Synchronous lesions occur in 6% of patients with colorectal carcinoma but rarely have a different or multiple-cell type [6]. No consensus guidelines are available for synchronous SCC and adenocarcinoma. We present a case of a multidisciplinary approach at an academic tertiary care center.
CASE REPORT
A 39-year-old man presented to an emergency department with proctalgia and hematochezia. He had a history of ulcerative colitis (UC) and of laparoscopic left colectomy 4 years prior for left colon adenocarcinoma (pT2pN0M0) at an outside institution.
Colonoscopy revealed inflammatory polyps and an ulcerated circumferential mass 30 cm from the anal verge and positive for SCC. Positron emission tomography/computed tomography showed radiotracer uptake in the colon anastomosis, transverse colon, inferior mesenteric artery stump and mesenteric lymph nodes (Figure 1). A 2-cm liver segment VIII lesion was positive for SCC on core needle biopsy (Figure 2).
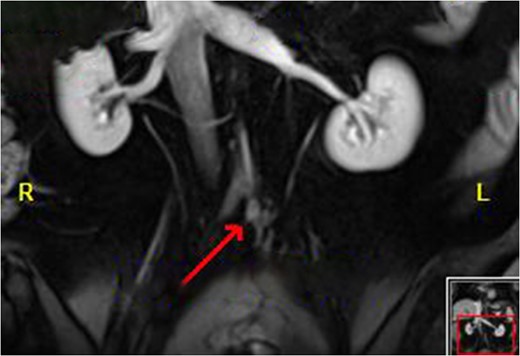
Disease of the inferior mesenteric artery stump. The arrow indicates the bulky disease.
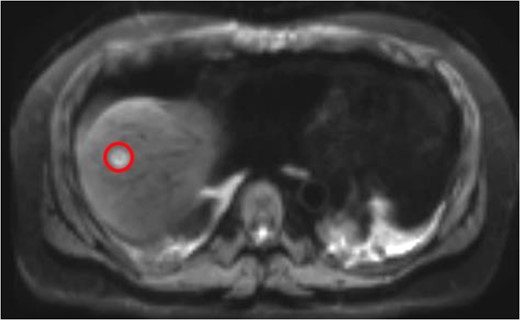
Liver Metastasis. The red circle indicates the 2-cm site of metastasis.
Neoadjuvant chemotherapy was initiated, ultimately consisting of two 3-week cycles of carboplatin and etoposide and four cycles of cisplatin and etoposide. The patient was then referred to our institution, where he underewent evaluation. His CEA and CA 19-9 levels were within the reference range.
Magnetic resonance imaging (MRI) after the initial chemotherapy cycle demonstrated a liver segment VIII 13-mm metastasis and indeterminate 5-mm lesions in segments VI and IV. Interventional radiology services performed a right portal vein embolization. On subsequent postembolization MRI, hepatic lesions were indiscernible, and liver remnant volumetrics increased from 21 to 35%.
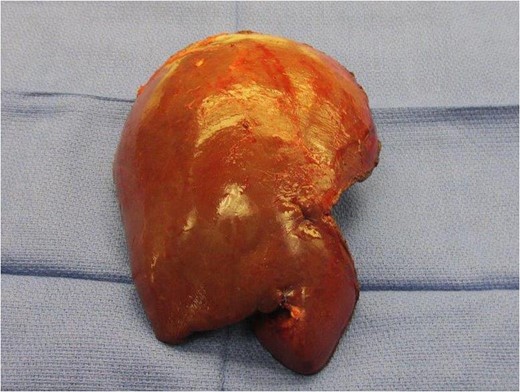
Neoadjuvant therapy was completed 1 month before surgical intervention. The patient underwent bilateral ureteral stents placement and an exploratory laparotomy in the lithotomy position. Intraoperative ultrasonography localized the tumor without showing any unexpected lesions. A right extended hepatectomy proceeded in the standard manner (Figs 3 and 4).
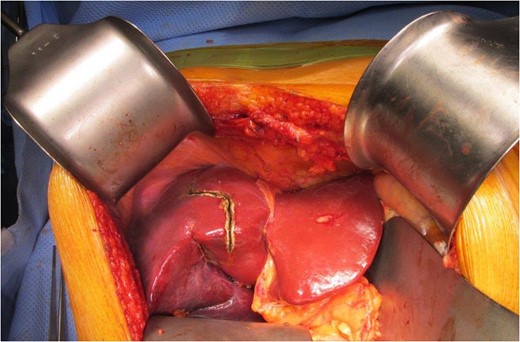
The colon was fully mobilized, and the mesentery was transected with high ligation of the ileocolic and middle colic pedicles. Because of the patient’s inferior mesenteric artery stump bulky disease, the surgeons performed a complete para-aortic lymphadenectomy and en bloc resection. The abdominoperineal resection was performed without incident. A pelvic drain was placed. His 15-day hospitalization was complicated by anemia requiring transfusions, lower-extremity deep vein thrombosis and prolonged ileus.
Liver pathologic evaluation revealed microscopic foci of metastatic adenocarcinoma in a background of necrosis in segment VIII without any additional lesions. Colon pathologic analysis showed a 5-cm tubulovillous adenoma with moderately differentiated adenocarcinoma. It also found high-grade SCC that infiltrated into pericolonic fat with lymphovascular and perineural invasion. A 4-cm tubulovillous adenoma with moderately differentiated adenocarcinoma was entering the muscularis propria. All margins were negative. Five of 20 lymph nodes were positive for SCC and adenocarcinoma (pT3pN2apM1a).
Adjuvant chemotherapy was delayed secondary to chemotherapy-induced cardiomyopathy with reduced ejection fraction. In the course of survivorship follow-up using the ASCRS/NCCN guidelines for resected metastatic adenocarcinoma, a 3-month MRI scan showed cancer recurrence in the liver, distinct from the resection area, and biopsy was positive for SCC [7]. Nivolumab therapy was started after a multidisciplinary discussion.
DISCUSSION
Published reports of colonic SCC and liver metastasis are rare [2, 4, 5, 8]. Nonetheless, the liver is the most common site of distant metastases from colonic SCC (incidence, 37.5–87.5%) [1, 4]. The treatment recommendation is subtotal proctocolectomy for patients with adenocarcinoma in the clinical setting of UC. The present patient was initially treated inadequately with a segmental left colectomy at the initial index operation. This initial procedure was performed at an outside institution, and therefore we became involved in the patient’s care at the second presentation. Although synchronous colectomy and hepatectomy for patients with metastatic colorectal cancer continues to be controversial, studies have shown its safety and improved efficiency for selected patients at medical institutions with adequate resources and experience [9]. This is the second case in the literature describing surgical resection for colonic SCC with liver metastases [8] and the first to describe a synchronous approach.
Despite the association of SCC with adenomas and an increased risk of malignancy with UC, we found only one publication describing synchronous SCC and adenocarcinoma in patients with UC and no publication describing management of synchronous SCC with recurrent adenocarcinoma and liver metastases [10]. Due to the limited number of cases, no consensus guidelines exist for colonic SCC. Limited reports have shown favorable results for patients treated with a platinum-based drug plus either etoposide or irinotecan [2, 4]. Radiation may also extend survival.
Adjuvant chemotherapy was delayed in the present case secondary to the patient’s cardiomyopathy and reduced ejection fraction. Had the patient not had cardiomyopathy, adjuvant chemotherapy would have been initiated sooner.
Additional research is needed to establish consensus guidelines for colonic SCC. We offer a novel example of synchronous resection of colonic primary and liver metastases after neoadjuvant etoposide and platinum-based chemotherapy. Despite excellent response to neoadjuvant therapy and young patient age, caution should be taken in surgical resection for SCC of the colon given the high risk of recurrence. This case vividly demonstrates that there is no substitute for impeccable surgical decision making. An oncologically appropriate proctocolectomy at the index operation would have eliminated the possibility of local recurrence or the development of an entirely different cancer. The biology of the cancer and the physiologic factors of the patient were ultimately not overcome by the multidisciplinary, aggressive medical and surgical approach, but they would have been easily prevented by appropriate surgical decision making at the index operation.
CONFLICT OF INTEREST STATEMENT
The authors have no conflicts of interest or sources of funding to report.
PATIENT CONSENT
Informed consent was obtained per hospital policy.
REFERENCES
- small cell carcinoma of lung
- ulcerative colitis
- adenocarcinoma
- hematochezia
- hepatic resection
- neoadjuvant therapy
- neoplasm metastasis
- surgical procedures, operative
- colon
- liver
- lymph nodes
- neoplasms
- liver metastases
- proctocolectomy
- squamous cell carcinoma, metastatic
- descending colon
- excision
- recurrence risk
- chemotherapy, neoadjuvant
- rectal pain



