-
PDF
- Split View
-
Views
-
Cite
Cite
Tohru Tanigawa, Hirokazu Tanaka, Fumiya Kano, Hiromi Ueda, Shigeru Inafuku, Nasal hemangiopericytoma successfully treated with a combination of rIL-2 and extranasal approaches, Journal of Surgical Case Reports, Volume 2017, Issue 10, October 2017, rjx202, https://doi.org/10.1093/jscr/rjx202
Close - Share Icon Share
Abstract
Hemangiopericytomas (HPCs) are uncommon vascular tumors originating from extracapillary cells called pericytes, and rarely occur in the nose or paranasal sinuses. We treated a 57-year-old man with nasal HPC who presented with nasal obstruction and hemorrhage. Nasal endoscopy showed a readily bleeding mass between the right nasal septum and inferior turbinate. Enhanced CT revealed a heterogeneous mass lesion with an enhancement effect that filled the right nasal cavity. A biopsy specimen was proved to exhibit a HPC histopathology. Recombinant interleukin-2 (rIL-2) was administered with a measurement of natural killer cell (NK cell) activity. Afterwards, wide excision with an extranasal approach was performed. The use of rIL-2 caused not only increased NK cell activity but also a reduction in the tumor size. With a combination of rIL-2 and wide excision with extranasal approaches, no local recurrence or metastasis has occurred over the last 4 years.
INTRODUCTION
Hemangiopericytomas (HPCs) are uncommon vascular tumors originating from extracapillary cells called pericytes, and rarely occur in the nose or paranasal sinuses [1]. The treatment of choice is a wide surgical excision. A high incidence of local recurrence (8–53%) and metastasis (35–57%) has been reported [1, 2]. There is no consensus about the efficacy of radiotherapy or adjuvant chemotherapy [2]. The role of immunotherapy has not been as well known. Therefore, a treatment strategy should be implemented as soon as possible.
Recombinant interleukin-2 (rIL-2: Imunase, Shionogi Pharmaceutical Co., Ltd., Osaka, Japan) is one of the cytokines produced from lymphocytes of human spleen by genetic engineering. It has been reported that natural killer (NK) cells amount to 15–20% of all lymphocytes, and decreased NK cell activity was shown in many patients with malignant tumors [3]. rIL-2 administration demonstrated not only activated NK cells but also anti-tumor effects in invitroexperiments [4]. Clinically, the safety and efficacy of rIL-2 have been reported for malignant vascular tumors [5]. However, the efficacy of rIL-2 against HPC has not been established.
In this report, we describe a case of nasal HPC successfully treated with rIL-2 and a local wide excision to obtain good visualization.
CASE REPORT
A 57-year-old man with a chief complaint of right nasal obstruction and hemorrhage was referred to our department for detailed examination. His own and family histories were unremarkable. Nasal endoscopy showed a readily bleeding mass between the right nasal septum and inferior turbinate (Fig. 1A). Enhanced CT (Fig. 2) revealed a heterogeneous mass lesion (5 × 1.7 cm) with an enhancement effect that filled the right nasal cavity. The nasal septum and lateral nasal wall were not deformed. Soft-tissue density was observed in the right ethmoid sinus, but was thought to be a mucous thickness due to its difference from the tumor’s density. The tumor evidenced an equivalent signal in the T1 and T2 weighted images of MRI with a strong enhancement effect.
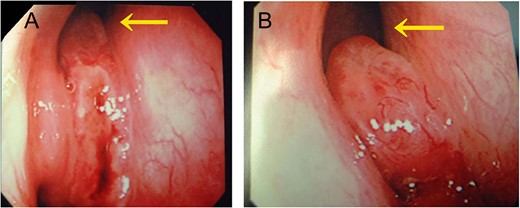
Endoscopic view of the right nasal cavity. (A) Before and (B) after rIL-2 administration. After rIL-2 administration, the tumor size was reduced (arrow).
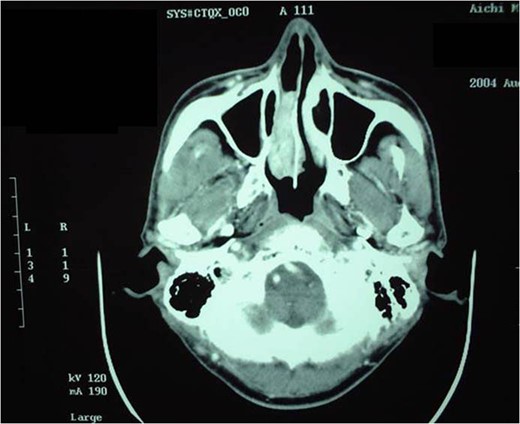
Enhanced CT before rIL-2 administration. A heterogeneous mass lesion with an enhancement effect filled the right nasal cavity.
A biopsy specimen was taken and the post-biopsy hemorrhage was able to be controlled by endonasal gauze packing. The tumor was proved to exhibit a HPC histopathology. The gallium scintigraphy was unremarkable.
We recommended a surgical resection as the therapy of choice, but the patient did not agree. Therefore, we decided to use rIL-2 which had been effective in a previous patient of ours with HPC of the maxillary sinus [6]. rIL-2 was given at a dose of 350 000 IU/day intravenously for 15 days, and a dose of 700 000 IU/day (twice a day) for more 5 days. No side effects such as fever elevation or eruption were seen. Nasal endoscopy showed that the pedicle of the tumor had become clearer because its size had been reduced (Fig. 1B). CT revealed a 46% size reduction (two-dimensional measurement) of the tumor. This result nearly corresponds to a partial response. However, since it was impossible to eliminate the tumor completely, the patient finally agreed to the operation.
Preoperative angiography (24 h before surgery) indicated that the blood supply originated mainly from a right infra-orbital artery. rIL-2 (350,000 IU) was administered from the distal portion of the maxillary artery. Afterwards, the maxillary artery was embolized super-selectively with an absorbent gelatin sponge.
An extranasal approach (lateral rhinotomy) was performed under general anesthesia. To obtain good visualization, the anterior wall of the right frontal sinus was also opened. The tumor had a pedicle on the right nasal septum near the olfactory cleft, which we extirpated totally, leaving an adequate free margin (Fig. 3A and B). The thick mucous recognized in the ethmoidal sinus proved to be non-malignant.
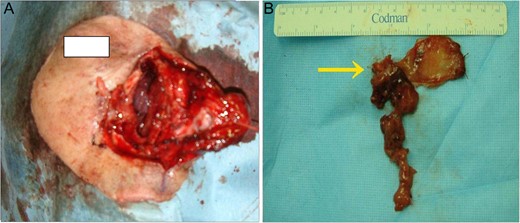
(A) After wide surgical excision (B) gross specimen. The tumor with a pedicle on the right nasal septum near the olfactory cleft was extirpated totally, leaving an adequate free margin. (arrow: pedicle of tumor).
Pathological examination showed that the proliferation of spindle-shaped pericytes had surrounded the ecstatic blood vessels to create a so-called ‘staghorn structure’ (Fig. 4). The vimentin and actin studies were positive, whereas negative results were obtained from studies on CD 34, S-100 protein and cytokeratin.
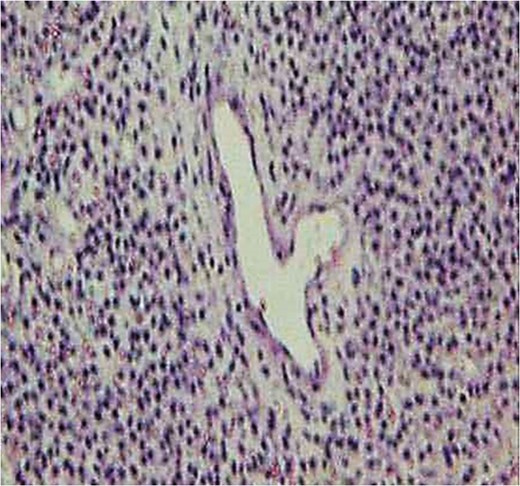
Pathological section (H-E staining). A proliferation of spindle-shaped pericytes surrounding the ectatic blood vessels to form a so-called ‘staghorn structure’ was shown.
The postoperative courses were uneventful, and no local recurrence or metastasis has occurred over the last 4 years.
Measurement of NK cell activity
Blood samples were obtained before and after intravenous administration of rIL-2. NK cell activity was measured using a 51Cr release assay employing K 562 erythroleukemia cell line as a target. The use of rIL-2 caused NK cell activity to increase from 28 to 37%.
DISCUSSION
In this report, we demonstrated that rIL-2 may be one of the useful treatments able to improve the poor prognosis of sinonasal HPC. HPC exhibits biologically malignant behavior, against which no effective combination of chemotherapy and radiotherapy has been established. Recently, the safety and efficacy of rIL-2 have been reported for angiosarcoma [5] of the skin and renal cell carcinoma [7]. rIL-2 is thought to attack the tumor cells directly as well as to activate the natural killer cells (NK cells), triggering the anti-tumor effects [5, 7]. In our case, after rIL-2 administration, increased NK cell activity and a reduction in the tumor size were also observed.
Patients receiving rIL-2 therapy may require management of severe side effects, especially cardiopulmonary and renal toxicities [8]. Other minor side effects include fever elevation, flu-like symptoms, fatigue, anorexia and skin eruption [8]. In our case, rIL-2 was given at a dose of 350 000 or 700 000 IU/day intravenously, and no side effects were seen. In the United States and Europe, total amounts of rIL-2 administration were 6–12 times as much as those in Japan [9]. High-dose rIL-2 administration could be the main cause of the frequently reported side effects.
Sinonasal HPCs are rare, with <200 cases reported in the literature [1, 10]. HPCs are clinically classified into two types depending on the prognosis. In the malignant type, the tumor tends to recur even after a wide surgical excision. On the other hand, in the benign type, the tumor does not recur. Although these categories exist, the natural history of the disease is not correlated with its histological grading, but remains rather unpredictable [1]. These facts indicate that HPCs should be treated as if they were malignant even when the potencial for proliferation is low.
In conclusion, since HPCs are uncommon vascular tumors and rarely occur in the nose or paranasal sinuses, further case studies are needed. Though treatment strategy has not been established, rIL-2 administration may be one of the useful treatments able to improve the poor prognosis of nasal HPC. The extranasal approach was necessary for good visualization and en bloc resection.
CONFLICT OF INTEREST STATEMENT
None declared.



