-
PDF
- Split View
-
Views
-
Cite
Cite
Yazan N AlJamal, Raaj K Ruparel, Steven R Jacobson, David R Farley, Maximum cosmesis for patients with primary hyperparathyroidism: a case for larger incisions, Journal of Surgical Case Reports, Volume 2017, Issue 10, October 2017, rjx193, https://doi.org/10.1093/jscr/rjx193
Close - Share Icon Share
Abstract
While minimally invasive parathyroidectomy is an advantage to many properly selected patients, longer incisions and even wide skin resection may be optimal in a select few. We present an 80-year-old woman with primary hyperparathyroidism and bothersome excess neck skin and subcutaneous fat. The parathyroid adenoma was easily excised through a vertically-oriented cervical excision that removed an ellipse of fat and skin. Midline wound closure with a small Z-plasty to avoid wound tethering facilitated a cosmetic closure well within the surgical capabilities of endocrine surgeons. This technique is useful for select patients and their surgeons and may avoid the expense of cosmetic surgery. We offer this controversial case to highlight the pros and cons of maximizing efficient surgical care to our endocrine surgery patients.
INTRODUCTION
Cervical exploration and parathyroidectomy cures over 95% of patients with primary hyperparathyroidism [1]. Although minimally invasive parathyroidectomy and limiting scar length is an advantage to properly selected patients, longer incisions and even wide skin resection may be optimal in a select few. We present a patient with primary hyperparathyroidism with excess skin laxity and bothersome subcutaneous fat in the cervicomental area.
CASE
An 80-year-old woman with multiple comorbidities presented with hypercalcemia. Her serum calcium level was 11.1 mg/dl (normal: 8.9-10.1) with a PTH of 100 pg/ml (normal: 10–65). Her urinary calcium was 251 mg/dl (normal: 100–400). A probable parathyroid abnormality in the left inferior neck was identified via a Sestamibi scan. Physical examination revealed an elderly woman with a large ‘turkey gobbler’ skin tag of the neck (Fig. 1). With the patient’s complaints of poorly fitting blouses and necklaces, endocrine and plastic surgeons discussed performing neck exploration as well as skin and subcutaneous tissue removal in one operation to prevent complications and to enhance cosmesis.

Elderly woman with a large ‘turkey gobbler’ skin tag of the neck.
SURGICAL APPROACH
Under general endotracheal anesthesia, the patient was prepared and draped with the neck extended. Due to excess skin laxity, an elliptical, vertically-oriented incision was made. Skin, fat and some platysmal muscle were removed. The midline strap muscles were separated through the median raphe and the thyroid gland identified. The left thyroid lobe was rotated medially, and a generous left inferior parathyroid gland was found. The blood supply was clipped and divided and the specimen removed. Pathologic and histologic analysis confirmed a parathyroid adenoma (190 mg). Intraoperative PTH monitoring showed a drop from 102 to 27 pg/ml in 10 min. The midline strap muscles were then loosely reapproximated with interrupted 3–0 Vicryl suture. The subcutaneous tissues were closed in layers with absorbable suture. Excess skin was displaced cephalad and the standing cones were excised (Fig. 2). To prevent tethering of the scar, a Z-plasty was performed at the mid portion. The incision was closed in layers with 3-0 and 4-0 Monocryl suture. A subcutaneous 10-French drain was placed. Sterile dressings of Steri-Strips and Dermabond were placed. The patient tolerated the procedure well. The drain was removed 24 h later. The scar healed nicely and the patient was happy with the results (Fig. 3). Serum calcium (9.0 mg/dl) and serum PTH (38 pg/ml) were normal at 6 months’ follow-up.
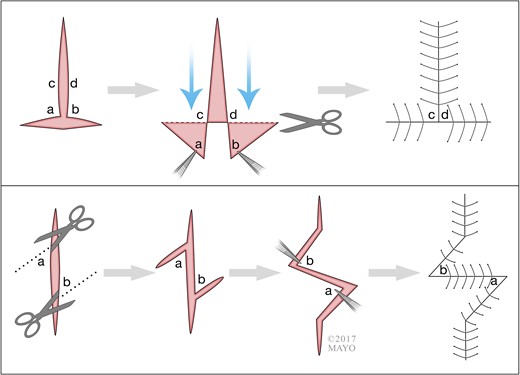
Upper: Burow’s triangles advancement flap. Lower: The 45-degree Z-plasty.

DISCUSSION
Skin and subcutaneous excision, parathyroidectomy, and complex skin closure can be performed concomitantly. In this elderly patient, the procedure was curative and cosmetic; it was simple, quick, safe, and effective. Additional operative time for this closure was ~15 min. The cost of one procedure compares favorably with performing parathyroidectomy and neck reconstruction in two separate procedures [2].
By advancing excess skin cephalad and excising Burow’s triangles, a surgeon is able to obtain tension-free closure of considerably large skin defects without dog-ear formation. Cosmetic surgery is expensive. General, endocrine and head and neck surgeons have the technical ability to safely resect an ellipse of skin and reapproximate the wound edges. Adding a Z-plasty to help avoid scar contracture is similarly not difficult.
Women, whether young or old, undergoing thyroid or parathyroid surgery frequently ask with a laugh, ‘Can you take out some fat at the same time?’ Our answer is ‘yes’ and all well-trained surgeons can safely do so in properly selected patients. We do not plan to charge patients for cosmetic surgery and expect that patient satisfaction will be sufficient payback for the additional 15 min of wound closure.
CONFLICT OF INTEREST STATEMENT
This manuscript has not been previously published or presented and is not being considered for publication elsewhere. All authors have read and approved the manuscript in its current form. No authors have any Conflict of Interest.



