-
PDF
- Split View
-
Views
-
Cite
Cite
Luis A Boccalatte, Juan Achaval Rodríguez, Axel Beskow, Demetrio Cavadas, Wright Fernando, Intussusception as a complication of bariatric surgery in pregnant patients: report of one case and revision of the literature, Journal of Surgical Case Reports, Volume 2017, Issue 10, October 2017, rjx189, https://doi.org/10.1093/jscr/rjx189
Close - Share Icon Share
Abstract
Occlusive complications after a laparoscopic Roux-in Y gastric bypass (LRYGB), appear mainly as fibrous membranes of wounds, internal hernias or intussusception. Intussusception after a bariatric surgery occurs in 0.1–0.3% of the cases. We present a case of intussusception in a pregnant patient after a LRYGB.
INTRODUCTION
Laparoscopic Roux-in Y gastric bypass (LRYGB) is currently one of the surgical options to treat morbid obesity. The occlusive post-LRYGB complications mainly appear as fibrous membranes of wounds, internal hernias or intussusception. Intussusception after a bariatric surgery occurs in 0.1–0.3% of the cases [1] and within the post-LRYGB OSBs (Obstruction of the small bowel), intestinal intussusception represents between 1 and 5% [2]. A bibliographical revision was made using Pubmed [laparoscopic Roux-en-Y gastric bypass AND Intussusception AND Pregnancy]. Five indexed works were found with six patients.
We present the case of a 32-year-old patient with 30-week gestation with a LRYGB performed in a different institution. We made a bibliographical revision of the current available literature.
CASE REPORT
The case of a 32-year-old female patient who is 30.6 weeks into her pregnancy (G2P1A0), hypertensive diabetic and dyslipidemic with a history of LRYGB with cholecystectomy associated to said procedure (due to symptomatic vesicular lithiasis) in 2011 in another medical facility.
She arrived at the Emergency Room of our hospital, after having been admitted in different institution, saying that 7 days ago she had started suffering from abdominal pain, muscle strain, nausea, bile-stained vomiting, negative catharsis and impossibility to release gases since the symptoms had started. During her previous hospitalization in the other facility, an upper gastrointestinal video endoscopy had been done where stenosis of the gastroyeyunostomy was discarded.
She had tachycardia as the only positive sign from the physical exam. Fetal vitality was confirmed via positive fetal heart beats (FCF: 147 beats per minute). A nasogastric tube was inserted with a 400 ml bilious charge.
In the multi detector computed tomography, evidence was seen on the left side of an image compatible with jejuno-jejunal invagination and an aerial image in halo that could correspond to pneumatosis of the invaginated loop (Fig. 1).
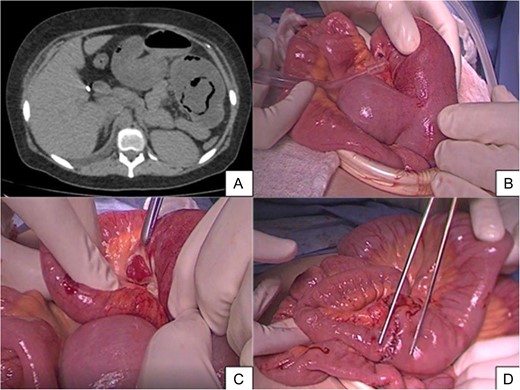
(A) Axial cross-section of MSCT without intravenous contrast where an aerial image is seen in halo which could correspond to pneumatosis and parietal swelling, image compatible with jejunojejunal invagination. (B) Intraoperative finding of intussusception. (C) The presence of necrosis in intussuscepted segment. (D) Jejunojejunal anastomosis is indicated with dissection tweezers.
A pneumoperitoneum with open technique was performed. In the laparoscopic work, abundant free liquid was seen in the abdominal cavity. Later, we identified the non-dilated loop (fine loop) at the level of the ileocecal valve and we explored the small bowel from distal to proximal to the foot of the Roux-in Y where no adherences involving this were seen. At 10 cm from the foot of the Roux-in-Y, we observed a retrograded intussuscepted jejunal segment, which had an intestinal perforation of one centimeter in diameter contained by the intussuscepted block.
Not managing to reduce the invagination using blunt manual techniques, we performed a mini-laparotomy. Once the enterotomy was done and the invaginated segment was reduced, we observed necrotic intussuscepted mucosa, performing a resection and termino-terminal jejunojejunal anastomosis at 4 cm from the foot of the Roux-in-Y (Fig. 2). Upon finalizing the procedure, we once again confirmed fetal vitality (FCF: 140 bpm).
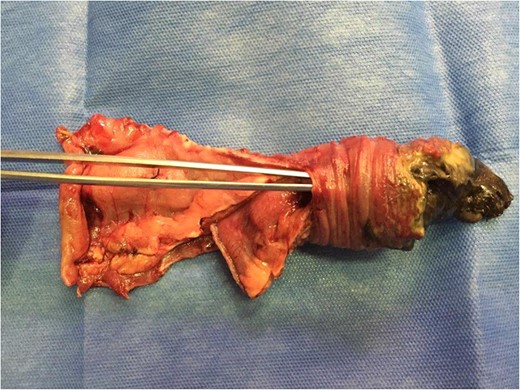
The dissection tweezers show the invaginated bowel segment. On the far right, an area of necrosis is seen with fibrine greenish streaks.
The diet advanced gradually with good tolerance, and she was discharged on the seventh day after the surgery.
DISCUSSION
LRYGB is currently one of the surgical options to treat morbid obesity. The occlusive post-LRYGB complications mainly appear as fibrous membranes of wounds, internal hernias or intussusception. OSB after LRYGB occurs with a frequency of 0.2–4.5% years or months after surgery [3, 4]. Among the OSBs, internal hernias represent the most common cause [1]. Intussusception as a complication of LRYGB occurs in 0.1–0.3% of the cases [1].
Pregnant patients constitute a special sub-population. Obese patients who wish to get pregnant, aside from the major reduction in post-surgical weight, and the resulting clinical improvements, improve their fertility [3]. Hyperemesis, nausea, reflux, the sensation of feeling full are frequent symptoms in the first trimester of the pregnancy. In a 30-week, pregnant patient with bile-stained vomiting with a history of LRYGB, an OSB must be suspected.
Post-LRYGB intussusception may be anterograde or retrograde. In most non-pregnant patients, retrograde intussusception is more frequent (75% [4]). In the six cases of post-LRYGB, pregnant patients reported in the literature [1, 5–8], the intussusception was retrograde. The foot of the Roux-in-Y was compromised in three cases, while the common loop was in the three remaining ones (Table 1).
| Author . | Year . | Country . | n = 7 . | BMI a/b (kg/m 2) . | Gestational (weeks) . | Time from LRYGB (years) . | Clinic manifestations . | Diagnosis . | Location . | Type . | Treatment . | Maternal mortality . | Infant mortality . |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Wax et al. | 2007 | USA | 1 | NR | 21 | 1 | Intermittent abdominal pain and vomiting | Intraoperative | Common loop | Retrograde | Reduction and resection | No | No |
| Tohamy et al. | 2009 | USA | 1 | NR | 33 | 4 | Epigastric pain and vomiting | CT scan | Distal foot Roux-in-Y | Retrograde | Reduction | No | No |
| Tuyeras et al. | 2012 | France | 1 | 34/52 | 17 | 4 | Epigastric pain and vomiting | Intraoperative | Jejunojejunal. Proximal foot Roux-in-Y | Retrograde | Reduction and resection | No | No |
| Renade et al. | 2013 | USA | 1 | NR | 33 | 10 | Epigastric pain and vomiting | CT scan | Common limb | Retrograde | Reduction and resection | No | No |
| Bokslag et al. | 2014 | England | 2 | 30/49 | 34 | 2,5 | Acute abdominal pain and nausea | Intraoperative | Jejunojejunal. | Retrograde | Resection | No | No |
| 25/NR | 24 | 9 | Acute abdominal pain and nausea | MRI | Distal foot Roux-in-Y | Retrograde | Resection | No | Yes (NNE*) | ||||
| Hospital Italiano | 2016 | Argentine | 1 | 28/41 | 30 | 4 | Intermittent abdominal pain and vomiting | CT scan | Distal foot Roux-in-Y | Retrograde | Resection | No | No* |
| Author . | Year . | Country . | n = 7 . | BMI a/b (kg/m 2) . | Gestational (weeks) . | Time from LRYGB (years) . | Clinic manifestations . | Diagnosis . | Location . | Type . | Treatment . | Maternal mortality . | Infant mortality . |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Wax et al. | 2007 | USA | 1 | NR | 21 | 1 | Intermittent abdominal pain and vomiting | Intraoperative | Common loop | Retrograde | Reduction and resection | No | No |
| Tohamy et al. | 2009 | USA | 1 | NR | 33 | 4 | Epigastric pain and vomiting | CT scan | Distal foot Roux-in-Y | Retrograde | Reduction | No | No |
| Tuyeras et al. | 2012 | France | 1 | 34/52 | 17 | 4 | Epigastric pain and vomiting | Intraoperative | Jejunojejunal. Proximal foot Roux-in-Y | Retrograde | Reduction and resection | No | No |
| Renade et al. | 2013 | USA | 1 | NR | 33 | 10 | Epigastric pain and vomiting | CT scan | Common limb | Retrograde | Reduction and resection | No | No |
| Bokslag et al. | 2014 | England | 2 | 30/49 | 34 | 2,5 | Acute abdominal pain and nausea | Intraoperative | Jejunojejunal. | Retrograde | Resection | No | No |
| 25/NR | 24 | 9 | Acute abdominal pain and nausea | MRI | Distal foot Roux-in-Y | Retrograde | Resection | No | Yes (NNE*) | ||||
| Hospital Italiano | 2016 | Argentine | 1 | 28/41 | 30 | 4 | Intermittent abdominal pain and vomiting | CT scan | Distal foot Roux-in-Y | Retrograde | Resection | No | No* |
BMI, Body mass index; BMI a, BMI before intussusception and BMI b, BMI after surgery. CT,computed tomography; NR, not reported.
*NNE, neonatal necrotizing enterocolitis.
| Author . | Year . | Country . | n = 7 . | BMI a/b (kg/m 2) . | Gestational (weeks) . | Time from LRYGB (years) . | Clinic manifestations . | Diagnosis . | Location . | Type . | Treatment . | Maternal mortality . | Infant mortality . |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Wax et al. | 2007 | USA | 1 | NR | 21 | 1 | Intermittent abdominal pain and vomiting | Intraoperative | Common loop | Retrograde | Reduction and resection | No | No |
| Tohamy et al. | 2009 | USA | 1 | NR | 33 | 4 | Epigastric pain and vomiting | CT scan | Distal foot Roux-in-Y | Retrograde | Reduction | No | No |
| Tuyeras et al. | 2012 | France | 1 | 34/52 | 17 | 4 | Epigastric pain and vomiting | Intraoperative | Jejunojejunal. Proximal foot Roux-in-Y | Retrograde | Reduction and resection | No | No |
| Renade et al. | 2013 | USA | 1 | NR | 33 | 10 | Epigastric pain and vomiting | CT scan | Common limb | Retrograde | Reduction and resection | No | No |
| Bokslag et al. | 2014 | England | 2 | 30/49 | 34 | 2,5 | Acute abdominal pain and nausea | Intraoperative | Jejunojejunal. | Retrograde | Resection | No | No |
| 25/NR | 24 | 9 | Acute abdominal pain and nausea | MRI | Distal foot Roux-in-Y | Retrograde | Resection | No | Yes (NNE*) | ||||
| Hospital Italiano | 2016 | Argentine | 1 | 28/41 | 30 | 4 | Intermittent abdominal pain and vomiting | CT scan | Distal foot Roux-in-Y | Retrograde | Resection | No | No* |
| Author . | Year . | Country . | n = 7 . | BMI a/b (kg/m 2) . | Gestational (weeks) . | Time from LRYGB (years) . | Clinic manifestations . | Diagnosis . | Location . | Type . | Treatment . | Maternal mortality . | Infant mortality . |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Wax et al. | 2007 | USA | 1 | NR | 21 | 1 | Intermittent abdominal pain and vomiting | Intraoperative | Common loop | Retrograde | Reduction and resection | No | No |
| Tohamy et al. | 2009 | USA | 1 | NR | 33 | 4 | Epigastric pain and vomiting | CT scan | Distal foot Roux-in-Y | Retrograde | Reduction | No | No |
| Tuyeras et al. | 2012 | France | 1 | 34/52 | 17 | 4 | Epigastric pain and vomiting | Intraoperative | Jejunojejunal. Proximal foot Roux-in-Y | Retrograde | Reduction and resection | No | No |
| Renade et al. | 2013 | USA | 1 | NR | 33 | 10 | Epigastric pain and vomiting | CT scan | Common limb | Retrograde | Reduction and resection | No | No |
| Bokslag et al. | 2014 | England | 2 | 30/49 | 34 | 2,5 | Acute abdominal pain and nausea | Intraoperative | Jejunojejunal. | Retrograde | Resection | No | No |
| 25/NR | 24 | 9 | Acute abdominal pain and nausea | MRI | Distal foot Roux-in-Y | Retrograde | Resection | No | Yes (NNE*) | ||||
| Hospital Italiano | 2016 | Argentine | 1 | 28/41 | 30 | 4 | Intermittent abdominal pain and vomiting | CT scan | Distal foot Roux-in-Y | Retrograde | Resection | No | No* |
BMI, Body mass index; BMI a, BMI before intussusception and BMI b, BMI after surgery. CT,computed tomography; NR, not reported.
*NNE, neonatal necrotizing enterocolitis.
The most accepted theories about the origin of post-LRYGB intussusception are based on ectopic pacemakers distal from the EEA with dilation of the foot of the Roux-in-Y as Hocking et al.[9] mentioned, which state that mechanical suture acts as a ‘lead point’ for the invagination [1, 8]. It is not known if the pregnancy per se increases the risk of intussusception or not, but it is suggested that the marked decrease in weight could generate an attenuated, less resistant and less ‘shock-absorbing’ mesentery of a possible process of twisting or intussusception [4, 7, 8].
The time between LRYGB and the appearance of the symptoms in the non-pregnant population is variable, generally between 1 and 3 years after surgery. The median manifestation time post-LRYGB was 4 years [r 1–10] and the mean gestational age was 27.42 weeks [r 17–34]. In terms of the symptoms, seven patients (including our case) presented intermittent abdominal pain, five acute, and two with several days in evolution. All of them had nausea.
The MSCT with contrast [2, 6, 7] confirms the diagnosis in 80% of the post-LRYGB pregnant patients and has minimal risks for fetal health and is considered in the study of choices [7]. In three cases [5–7], the diagnosis was intraoperative. In two cases [1, 7], the abdominopelvic MSCT did not require the contrast phase for the definitive diagnosis and in one case, the diagnosis was done using magnetic resonance imaging (MRI; Table 1) [5].
The delay in surgical intervention in OSB can increase the fetal maternal morbimortality. Surgical treatment within 48 h of the clinical picture has 10% mortality, while after 48 h of the diagnosis, the mortality rises to 50% [10]. Only one neonatal death has been reported due to necrotizing enterocolitis (NEC) associated to maternal pneumonia [5].
The surgical treatment alternatives (Table 1) consist in the reduction [1], reduction plus resection or IR (intestinal resection) plus EEA0 [5, 9]. In our case, the IR plus EEA decision was made because of the necrosis of the intussuscepted block.
CONFLICT OF INTEREST STATEMENT
None declared.
FUNDING
None.
CONSENT
Consent was obtained from the patient for publication.
ETHICAL APPROVAL
Ethical approval and informed consent were obtained and available upon request.
AVAILABILITY OF DATA AND MATERIALS
Data are available from the medical record of Institution. The data cannot be publicly available due to local legal restrictions.



