-
PDF
- Split View
-
Views
-
Cite
Cite
Kemal M Tekeli, Keith Altman, Longstanding unilateral dislocation of the temporomandibular joint in a 6-year-old girl, Journal of Surgical Case Reports, Volume 2017, Issue 10, October 2017, rjx187, https://doi.org/10.1093/jscr/rjx187
Close - Share Icon Share
Abstract
Unilateral longstanding dislocation of the temporomandibular joint (TMJ) is rare in children. These patients may demonstrate some function in opening and closing of the mouth due to the formation of a pseudo-joint in the dislocated position. In this report we describe a case of longstanding unilateral dislocation of the TMJ in a 6-year-old girl, highlighting the diagnostic difficulty and management of the condition.
INTRODUCTION
Temporomandibular joint (TMJ) dislocation is defined as displacement of the mandibular condyle anterior to the articular eminence so it no longer sits within the glenoid fossa [1]. Longstanding dislocation is a rare condition for which the terminology and management are not clear. It can be defined as any dislocation existing more than a month [1]. However, recently, it was described as acute dislocation which was either inadequately treated or left untreated more than 72 h [2]. We describe a case of longstanding unilateral dislocation of the TMJ in a 6-year-old girl.
CASE REPORT
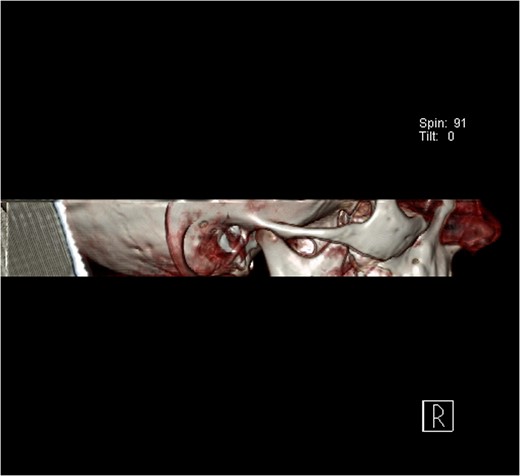
A 6-year-old girl presented to the Emergency Department with a suspected mandibular dislocation after falling off her scooter. She was previously fit and well with no significant medical history. She had complete restriction of all mandibular movements and trismus. The dental occlusion demonstrated a cross-bite with all the posterior teeth in contact and a mandibular asymmetry with the chin significantly deviated to the left side. Radiographic investigations (orthopantomogram (OPG) and postero-anterior (PA) mandible images) were performed but confirmation of the dislocation could not be determined on these views (Fig. 1). Consequently, a computerized tomography (CT) scan was performed that confirmed significant displacement of the condyle anteriorly and superiorly into the infratemporal fossa (Fig. 2). In addition calcification of the lateral and medial pterygoid muscles was noted on the affected side indicating chronic nature of the condition. Discussion with the patient’s general dental practitioner (GDP) revealed that the patient had a pre-existing dental malocclusion comprising of a cross-bite and mandibular asymmetry and this was also corroborated by a photograph taken well before the scooter accident. On this evidence it was therefore presumed that the condyle had been dislocated for many months or years and the scooter accident had only highlighted this. There were no other traumatic events of note in the history. The TMJ could not be convincingly reduced via a Hippocratic manoeuvre under a short general anaesthetic despite several attempts. In order to re-image the TMJ a magnetic resonance imaging scan was performed to prevent additional irradiation. This scan confirmed that the TMJ was still dislocated and had not been reduced. Due to the unsuccessful closed reduction, it was decided to perform an open reduction via a Risdon incision. When reduction with traction wires at the mandibular angle failed a bone hook was placed into the sigmoid notch and the dislocation was reduced using a fair degree of force.
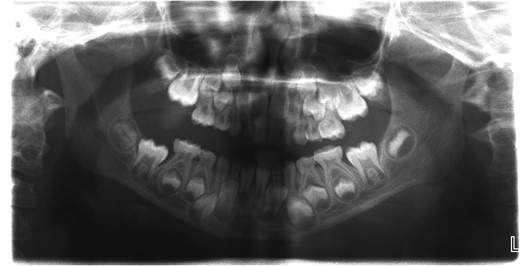
Orthopantomogram (OPG) of the patient with longstanding dislocation.

Computerized tomography (CT) scan of the dislocated left temporomandibular joint.
Computerized tomography (CT) image of the normal right temporomandibular joint.
DISCUSSION
This case is unique due to the rarity of the longstanding unilateral jaw dislocation. A systematic review comparing 425 cases of TMJ dislocation identified only four cases to be unilateral, and only 35 to be longstanding [3]. Another review revealed 37 cases of longstanding TMJ dislocation; one of which was a paediatric case [4]. In case series of Caminiti and Weinberg, a 16-year-old girl with prolonged dislocation was also highlighted [5].
This case highlighted that an OPG is not always adequate to confirm the diagnosis if clinically it is not clear that there is a dislocation, especially when it is chronic and the occlusion has developed to accommodate the new mandibular position. Longstanding TMJ dislocations tend to be more complex to treat. This is generally due to calcification of the pterygoid muscles [6]. Huang et al. proposed a treatment strategy classifying longstanding dislocations according to their duration. For dislocations <3 weeks, a closed reduction was proposed. For longstanding dislocations from 1 to 6 months open reduction with wide subperiosteal dissection and use of traction wires and retractors was suggested. For dislocations longer than 6 months, other additional techniques may be required including condylectomy, condylotomy, myotomy and arthroplasty [2, 7]. A chronically dislocated TMJ often results in changes to the occlusion and muscular posture, particularly in the growing patient. Consequently patients will require orthodontic assessment following initial management [8].
CONCLUSION
Longstanding dislocation of TMJ in paediatric population is very rare. One of the reasons may be underreporting due to the diagnostic pitfalls. The authors recommend that all children in whom the clinical diagnosis is in doubt should have a CT or an MRI scan. In paediatric population, OPG is not adequate for radiological diagnosis.
CONFLICT OF INTEREST STATEMENT
None.
FUNDING
None.



