-
PDF
- Split View
-
Views
-
Cite
Cite
Stefanie M Croghan, Orla McCormack, Anna L Walsh, Ted McDermott, Ascending cholangitis: rare presentation of a ruptured right-sided renal angiomyolipoma, Journal of Surgical Case Reports, Volume 2017, Issue 10, October 2017, rjx191, https://doi.org/10.1093/jscr/rjx191
Close - Share Icon Share
Abstract
We report the case of a 46-year-old female who presented to the Emergency Department with acute, painful obstructive jaundice, with evidence of secondary ascending cholangitis. Surprisingly, imaging revealed the clinical picture to be caused not by hepatobiliary pathology, but by external compression of the biliary tree from a ruptured renal angiomyolipoma (AML) of the right kidney. The patient remained haemodynamically stable and conservative management saw resolution of biliary obstruction. We believe this to be the first report of a renal AML presenting in this way. This report highlights the diverse spectrum of presentations of renal angiomyolipomas.
INTRODUCTION
Renal angiomyolipomas are typically found incidentally or present with pain, haematuria or a palpable mass. However, unusual presentations have been reported, especially in the context of tumour rupture. We present what we believe to be the first case in the literature of an ruptured renal angiomyolipoma (AML) presenting with biliary obstruction. This report outlines the potential of renal AMLs to present atypically, and demonstrates an apparently straightforward clinical presentation with an unusual aetiology.
CASE
A 46-year-old female with a distant history of cholecystectomy presented to A&E reporting right upper quadrant (RUQ) pain and jaundice of 5 days duration. She reported the onset of fevers and vomiting the previous day. There were no bowel or urinary symptoms.
On examination, she was apyrexial with scleral icterus. Her abdomen was soft but tender in the RUQ. Investigations revealed Hb of 10 g/dL, leukocytosis (14.6 × 109/L) and elevated C-reactive protein (299 mg/L). Liver function tests were elevated in an obstructive pattern, with bilirubin 46 umol/L, alkaline phosphatase 274 IU/L and gamma glutamyl transferase 142 IU/L. Renal function was normal.
Fluid resuscitation and IV antibiotics were commenced, and an abdominal ultrasound performed. It revealed the presence of a large heterogenous right renal mass. Further evaluation was performed with magnetic resonance cholangiopancreatography. Findings were of a 5.7 × 4.6 cm2 exophytic mass of high T1 signal intensity arising from the posterior right kidney. Adjacent to the mass was a large 8.3 × 10 cm2 retroperitoneal haematoma (Fig. 1). These findings were consistent with a ruptured angiomyolipoma. The adjacent common bile duct was dilated at 8 mm, secondary to mass effect (Fig. 2).
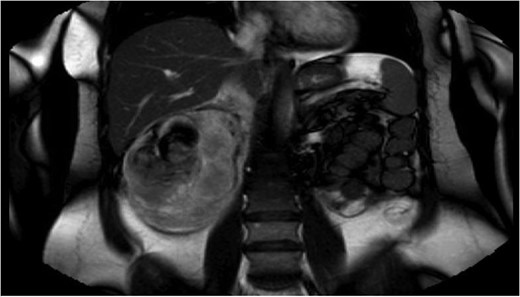
Magnetic resonance cholangiopancreatography (MRCP) on admission, showing an exophytic mass arising from posterior right kidney, with adjacent 8.3 × 10 cm2 retroperitoneal haematoma.
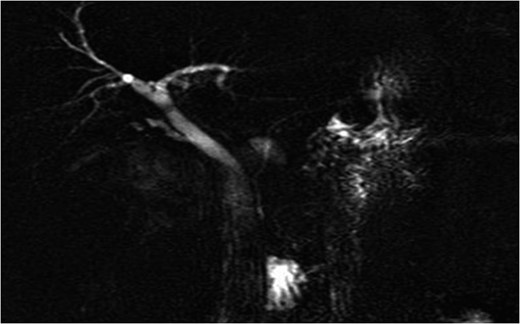
Admission imaging revealing dilatation of the common bile duct (8 mm), due to external compression.
The case was discussed at urology MDT for possible selective renal embolization, however, in the context of improving clinical status, conservative management with observation was chosen. The patient remained afebrile and haemodynamically stable, and pain resolved. Over 3 days, bilirubin reduced to 25 umol/L, with stable Hb and renal function. Repeat ultrasound showed reduction in size of the retroperitoneal haematoma and normalization of bile duct calibre.
The patient was discharged on Day 4. Bloods repeated at 1 week were reassuring. At follow-up 3 months later, haemoglobin was 14.7 g/dL and liver function tests had normalized, with bilirubin of 9 umol/L. CT urogram showed reduction in size of the ruptured angiomyolipoma, with overall size of AML and haematoma measuring measured 9 × 6.5 cm2 as compared to 17 × 10 cm2 on presentation. Conservative management was continued, due to stability and patient preference, with follow up plan to re-image at 3 monthly intervals, alternating CT with ultrasonography, with consideration of selective angioembolization should further complications occur.
DISCUSSION
This unusual case prompted us to review the documented presentations of renal angiomyolipomas, and management strategies.
Trends in presentation and diagnosis of renal angiomyolipomas appear to be changing. A 2002 literature review [1] and Egyptian 2008 retrospective study (n = 60) [2] showed flank pain to be the most common presenting feature of renal AML (41–50%), followed by haematuria (11–21.7%) or a palpable mass (11%).
More recent studies highlight a shift towards incidental presentations, likely a consequence of increased availability and sophistication of imaging performed for other indications, or as a screening modality in tuberous sclerosis. A retrospective UK study published in 2011 noted 86% of patients (n = 102) to be asymptomatic at diagnosis of AML. Those with symptomatic presentations had pain (5.9%), haematuria (2.9%) or spontaneous life-threatening haemorrhage (5.9%). Patients with tuberous sclerosis were noted to be more frequently asymptomatic at diagnosis; possibly reflecting a referral bias [3].
A 24-year US study concluded in 2009 with similar results; 83.9% of patients (n = 87) presented incidentally, while 16% were symptomatic with pain, haematuria or haemorrhage [4].
Less commonly, renal angiomyolipomas present as the eponymous Wunderlich’s syndrome, first described in 1856, with spontaneous rupture resulting in haemorrhage confined to perirenal/subcapsular spaces [5]. The literature also reveals a handful of apparently unique cases, including presentation as thrombus involving the right atrium [6], caudal rupture resulting in haemoperitoneum with abdominal compartment syndrome [7] and duodenal obstruction [8].
Our patient was managed with close clinical observation as an inpatient during the acute phase, and subsequently discharged on active surveillance. Management strategies for renal AMLs have been somewhat controversial, with debate regarding whether a particular tumour size threshold (usually 4 cm) serves as an absolute indication for intervention in the absence of symptoms or concern for malignancy. Recent studies suggest safety of active surveillance for asymptomatic renal AMLs > 4 cm [9] and those in the 4–6 cm bracket [10]. Whilst higher rates of requirement for delayed intervention are acknowledged with larger tumours, this approach potentially avoids overtreatment of a significant proportion of patients [9].
Renal angiomyolipomas are interesting tumours with a diverse array of potential presentations. Our case of an AML presenting as biliary obstruction further reiterates this potential to present atypically.
CONFLICT OF INTEREST STATEMENT
None declared.
FUNDING
None.
PATIENT CONSENT
Yes.



