-
PDF
- Split View
-
Views
-
Cite
Cite
Dafney L. Davare, Zishan Chaudry, Rafael Sanchez, Seong K. Lee, Chauniqua Kiffin, Andrew A. Rosenthal, Eddy H. Carrillo, A unique case of venous air embolus with survival, Journal of Surgical Case Reports, Volume 2016, Issue 9, September 2016, rjw153, https://doi.org/10.1093/jscr/rjw153
Close - Share Icon Share
Abstract
Venous air embolus (VAE) occurs when gas, specifically atmospheric air, enters into the vascular system. Although rare, they can be fatal due to risk of cardiovascular collapse. In this report, we present a unique case of a 66-year-old female trauma patient with an inferior vena cava air embolism. An overview of the potential cause is presented, along with a review of the management of VAE.
Introduction
Venous air embolus (VAE) is a rare event with lethal consequences. The presentation of this phenomenon can vary widely with a multitude of nonspecific signs. We present the case of a 66-year-old female patient found to have air within the inferior vena cava (IVC), right iliac and femoral veins. Furthermore, we review the current literature regarding diagnosis and treatment of VAE. Immediate identification and management are key to patient outcomes. It is critical that the clinician understand the pathophysiology of this disease process and how it relates to the current treatment recommendations.
Case Report
A 66-year-old female patient presented to our level I trauma center after a motor vehicle collision. She sustained multiple injuries including several fractured ribs, hemopneumothorax and a right diaphragmatic rupture. She was hemodynamically normal during her primary and secondary survey, and received a right femoral vein central venous catheter (CVC) for fluid resuscitation. She underwent computed tomography (CT) scan for further diagnostic evaluation and was noted to have the aforementioned injuries and a significant amount of air within the IVC, right iliac and femoral veins (Figs. 1–3). She was immediately placed in Trendelenburg position; a new subclavian CVC was inserted and used to withdraw air. Her right femoral vein introducer was suspected to be the source and was removed. She remained stable with no obvious clinical sequelae and underwent operative repair of her diaphragmatic injury. The patient was discharged on hospital Day 10 with no issues.

Axial contrast-enhanced CT image of the abdomen demonstrating air within the IVC (arrow).

Axial CT image of the pelvis demonstrating the CVC (white arrow) with adjacent air (red arrow) in the right external iliac vein.
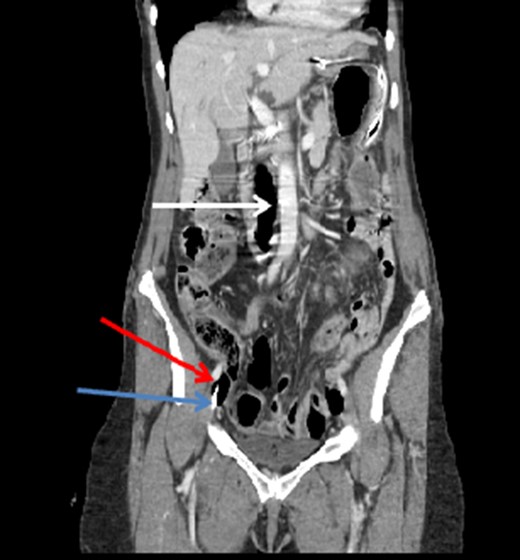
Coronal CT image of the abdomen and pelvis showing a significant amount of air within the IVC (white arrow). Note the CVC (blue arrow) and additional air (red arrow) in the right external iliac vein.
Discussion
VAE occurs when air or gas enters the vascular system [1, 2]. This is a rare but fatal event with an unknown incidence rate [1, 3–5]. The mortality rate ranges from 48% to 80% [1, 5].
The development of VAE requires an entry point into the venous system and a pressure gradient promoting the movement of gas into the system [1, 2, 6]. The most commonly recognized scenario for VAE is during insertion or removal of a CVC [1, 3, 6, 7]. Other causes include penetrating chest trauma, orthopedic surgery, laparoscopic surgery, neurosurgical and head and neck procedures [1, 6, 8]. There has also been literature on the development of VAE in scuba divers during their ascent in water [5].
VAE is not easily recognized as symptoms are nonspecific and mimic cardiac, neurological and pulmonary diseases. Presentation can range from no clinical signs to sudden cardiovascular collapse [1, 3, 8]. Signs and symptoms include dyspnea, tachyarrhythmias, hypotension, chest pain and cough [1, 8]. Mechanically-ventilated patients can develop hypoxemia and a sudden decrease in end-tidal carbon dioxide (ETCO2) [2, 8]. The severity of the patient's presentation is dependent on the volume of air, the rate at which air accumulates in the vascular system, the type of gas involved and the location of the embolus [1, 2]. Mirski et al. have described the lethal dose of vascular air to be 3–5 ml/kg with a lethal rate of 100 ml/sec [1, 2]. Furthermore, a significant amount of air can become lodged within the right ventricle and cause a ventricular outflow tract obstruction [1, 2, 8]. This contributes to right sided heart failure and death. VAE can also enter into the arterial circulation, causing a paradoxical embolus [1, 6, 8]. This may occur in patients with a patent foramen ovale, present in 20–35% of the population [1–3, 8]. When gas enters into the arterial circulation the resulting signs and symptoms reflect end organ ischemia.
Physical examination of a patient with a VAE may reveal nonspecific findings such as wheezes, rales or a mill-wheel murmur on cardiac auscultation [6]. Chest radiography (CXR) findings are also nonspecific. Findings of pulmonary edema on CXR in the setting of recent CVC insertion, removal or neurological surgery may increase suspicion for VAE. Another method for diagnosis is the transesophageal echocardiogram (TEE) [1, 8]. Although invasive, TEE is the most sensitive diagnostic test, and can identify as low as 0.02 ml/kg of air [2, 5, 8]. Precordial Doppler ultrasound is also useful and noninvasive [2]. Compared to the TEE, the Doppler is less sensitive and can identify 0.05 ml/kg of air [2]. Other less sensitive means for diagnosing VAE include ETCO2 monitoring, esophageal stethoscope and the pulmonary artery catheter [2, 5].
The key to management of VAE is prevention and early identification. A high clinical suspicion is important for those patients undergoing procedures with high VAE incidence. Patient positioning for procedures such as CVC insertion has been reported as a means for decreasing VAE risk [2, 3]. Placement of a patient in Trendelenburg and encouraging the Valsalva maneuver during insertion have been recommended for minimizing VAE incidence [2–4]. Avoiding hypotension can decrease the pressure gradient promoting air entry by increasing venous pressure [2].
When VAE is identified or suspected, the clinician must prevent further accumulation [4]. This can be accomplished by occluding the surgical point of gas entry with saline-soaked dressings [2].
Patients presenting with dyspnea and hypoxia require supplemental oxygen, or mechanical ventilation. Oxygen aids in decreasing embolus size by removing nitrogen (nitrogen washout) [1, 2, 6, 8].
Another treatment recommendation involves decreasing the right ventricular outflow obstruction, by placing the patient in Trendelenburg position or the partial left lateral decubitus position [2]. Although described throughout literature, this remains controversial in improving the hemodynamics associated with VAE.
Air aspiration through venous catheters inserted into the right heart has been suggested as another option in management [4, 5, 8].
Finally, hyperbaric oxygen therapy (HBOT), which has been used in divers suffering from air emboli, is a valuable tool for treatment of VAE. HBOT can attenuate the size of the embolus through more rapid nitrogen washout and improve tissue oxygenation [2, 6]. This treatment requires transfer of the patient to a facility that has HBOT, and therapy must be instituted within 5 hours.
Once diagnosed, VAE can be difficult to treat. Supportive care and promotion of nitrogen washout through oxygen administration or HBOT are most successful [1, 2, 6, 8]. Positioning is the mainstay of initial management, despite controversy in its success [2, 4].
In our case, the VAE was due to a defect within the CVC allowing venous air entry. The patient had no clinical signs or symptoms despite the CT scan findings. She was immediately managed with repositioning and CVC aspiration and suffered no clinical sequelae.
Conflict of Interest Statement
None declared.



