-
PDF
- Split View
-
Views
-
Cite
Cite
Wei-Chen Chen, Chih-Hsuan Changchien, Yu-Min Su, Bipaddled anterolateral thigh perforator flap for simultaneous reconstruction of bilateral buccal defects following oral cancer ablation or release of oral submucous fibrosis, Journal of Surgical Case Reports, Volume 2016, Issue 9, September 2016, rjw154, https://doi.org/10.1093/jscr/rjw154
Close - Share Icon Share
Abstract
It is a challenge to simultaneously reconstruct bilateral buccal defects following oral cancer ablation or release of oral submucous fibrosis. In this study, we report two cases where bipaddled anterolateral thigh perforator flaps were used to resurface two separate buccal defects.
Introduction
Trismus can be caused by severe oral submucous fibrosis (OSF), and surgical release remains the treatment of choice. Free tissue transfer appears to be an alternative and effective option to provide sufficient soft tissue volume and greater freedom to reconstruct defects of any size and in any location. However, double free flap transfers for reconstruction of two separate buccal defects requires a second microvascular anastomosis and longer operation time. In this study, we used a bipaddled design, which precludes the need for a second free flap and does not require a second microvascular anastomosis.
Case Reports
Case 1
A 48-year-old man had suffered from left buccal mucosa verrucous hyperplasia with moderated dysplasia following wide excision and split-thickness skin graft. He presented with progressive limitation of mouth opening for about 6 months’ duration, and the preoperative interincisor distance (IID) was 5 mm. Following excision of submucous fibrosis, coronoidotomy and myotomy, the IID increased to 32 mm (Fig. 1). A bipaddled anterolateral thigh (ALT) perforator flap was harvested (Fig. 2). A gingivolabial sulcus incision was made, and the bridged pedicle merged into the subcutaneous layer of the lower lip. The left facial recipient vessels were used, and the donor site was closed primarily. The IID was 25 mm at the 4-month follow-up (Fig. 3).
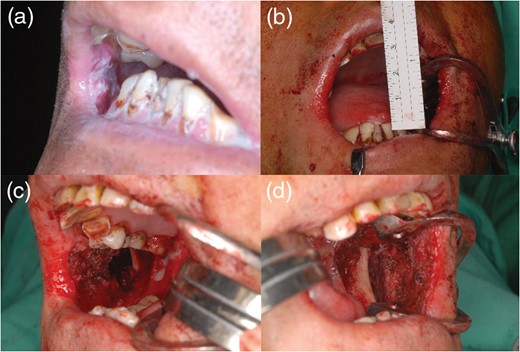
Case 1. (a and b) A 48-year-old man presented with severe trismus with preoperative and intraoperative IIDs of 5 and 32 mm, respectively (c and d). After release of submucous fibrosis, the right buccal defect was 8 × 4 cm and the left buccal defect was 9 × 6 cm.
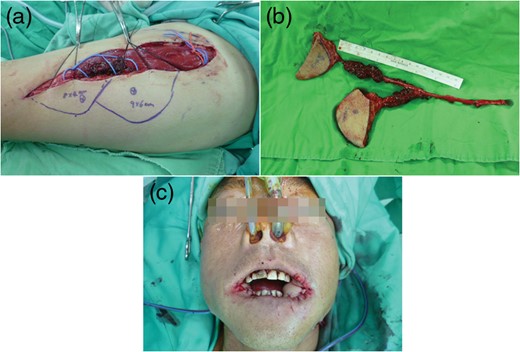
Case 1. (a and b) Bipaddled ALT perforator flap was harvested from the descending branch of the lateral circumflex femoral artery. Bridged pedicle length was 8 cm, and the common mother vessel length was 10 cm. (c) Intraoperative appearance after flap was placed on both sides.
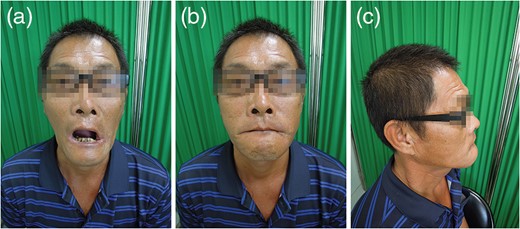
Case 1. (a) The IID was 25 mm at the 4-month follow-up. (b and c) Anterior and lateral views showed inward displacement of the lip.
Case 2
A 47-year-old man presented with bilateral buccal squamous cell carcinoma with an IID of 15 mm. Following tumor ablation and trismus release (Fig. 4), these defects were resurfaced with bipaddled ALT perforator flaps. The bridged pedicle was placed through a gingivolabial sulcus incision. The left superior thyroid artery was used as a recipient vessel, and the donor site was closed primarily. Secondary de-bulking of the flaps and commissuroplasty were performed, and the IID was 25 mm at the 7-month follow-up (Fig. 5).
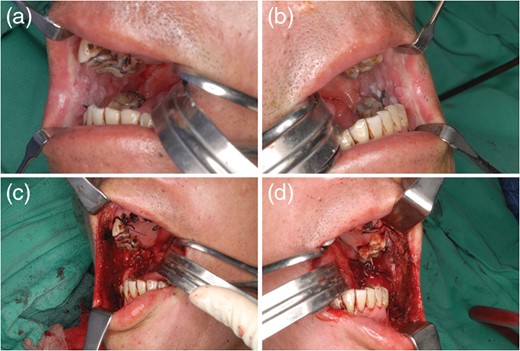
Case 2. (a and b) A 47-year-old man had bilateral buccal squamous cell carcinoma with an interincisal distance of 15 mm. (c and d) Following tumor ablation and the release of trismus, bilateral buccal defects were 10 × 7 cm and 10 × 7 cm, respectively.

Case 2. (a) Intraoperative appearance after reconstruction with bipaddled ALT perforator flap. (b) This image showed bulky flap after 1.5 months’ follow-up. (c) The patient received secondary de-bulking and commissuroplasty 3 months after reconstruction. (d) Appearance of the patient at the 7-month follow-up.
Discussion
OSF is a chronic disorder with progressive fibrosis of the submucosal tissue. The fibrotic bands restrict mouth opening leading to deterioration in nutritional intake, speaking and dental hygiene. The treatment of patients with OSF depends on the degree of trismus, which has been classified by Khanna and Andrade [1]. There are many techniques to resurface soft tissue defects. Secondary healing or skin grafting have been disappointing because of subsequent contracture formation and rebound trismus. Vascularized tissue transfer using a local or free flap provides an effective option to minimize trismus recurrence. However, resurfacing the defects with various local flaps has several limitations. Tongue flaps are too bulky and need secondary surgical division. Buccal fat pads are a simple method because access is easy, but they usually cannot reach the anterior part of the defect. The nasolabial flap also has limited donor tissue, and the main disadvantage was the dissatisfaction with extraoral scars and intraoral growth of hair. Free tissue transfer seems to be an effective option to provide sufficient soft tissue volume and greater freedom to reconstruct any defect size in any location.
A free radial forearm flap is widely used to cover buccal defects after trismus release, because of its excellent vascularization, thinness and pliability. The work of Wei advocated reconstruction using two free forearm flaps from bilateral or single forearms and achieved good outcomes [2, 3]. Lee et al. developed a bipaddled radial forearm flap from one forearm donor site to avoid second microvascular anastomosis [4]. However, disadvantages of the radial forearm flap include unsightly scar formation over the forearm and often the skin needs grafting close the recipient site, unless the flap is quite small. The sacrifice of one or both radial arteries may result in potential circulatory compromise to the hand, especially in heavy smokers.
Recently, free ALT flaps have gained popularity for head and neck reconstruction. The popularity of the workhorse ALT flap is owing to its long vascular pedicle, large skin paddle and decreased operative time with a two-team approach. Huang et al. proposed two independent ALT flaps from one thigh [5]. The two separate flap method undoubtedly needs two recipient vessels and demands a longer operation time for second microvascular anastomosis. Chen et al. developed a cross-cheek ALT flap with bilateral skin paddles and a palatal bridge [6], and this technique needs only one recipient vessel. However, removal of the palatal mucosa to accommodate the bridging segment of the cross-cheek flap has the potential need for skin grafting for donor site closure.
We report two cases who received successful reconstruction using bipaddled ALT perforator flaps. This technique has the following advantages. First, harvesting two ALT flaps from single donor site to cover two separate buccal defects precludes the need for additional recipient vessels for a second free flap and this decreases operating time and donor site morbidity. More free flap donor sites and recipient vessels can be preserved for future use in salvage or reconstruction after oral cancer recurrence. Second, the common pedicle length of the ALT flap is sufficiently long to reach recipient vessels in the neck. Third, the donor sites are usually closed primarily when the defect is <6–8 cm wide, and the scar can be easily hidden by short pants. Lastly, the sacrifice of the descending or transverse branch of the lateral circumflex femoral artery and the compromise of lower limb circulation have not been reported.
There are some limitations of this surgical technique. First, the major concern is regarding the bulkiness of ALT flap. To overcome this dilemma, we can create a deeper buccal pocket during submucous fibrosis excision or perform a flap-thinning procedure. Second, mouth opening exercises are recommended to start as soon as possible after trismus release (1–3 days), and care must be taken to avoid bridged pedicle compression. Another concern is postoperative shallow gingivolabial sulcus that causes inward displacement of the lip and drooling, and may need secondary correction for deepening of the gingivolabial sulcus.
In summary, using a bipaddled ALT perforator flap is an ideal surgical strategy to simultaneously reconstruct bilateral buccal defects, and more free flap donor sites and recipient vessels are preserved for future use in salvage or reconstruction.
Conflict of interest statement
None declared.



