-
PDF
- Split View
-
Views
-
Cite
Cite
Hana Kennedy, Jayanth Kunjur, Kavita Amarasinghe, Graham Smith, Extramammary Paget's disease of the oral tissues—literature review and a rare case report, Journal of Surgical Case Reports, Volume 2016, Issue 9, September 2016, rjw152, https://doi.org/10.1093/jscr/rjw152
Close - Share Icon Share
Abstract
Extramammary Paget's disease (EMPD) is a rare, cutaneous adenocarcinoma in situ characterized by a chronic eczema-like rash of the anogenital regions. It is usually slow growing, locally invasive and presents mainly with pruritis. Extremely rare in the oral tissues, here we present a case of EMPD of the hard palate and a review of the existing literature base.
Introduction
Paget's disease (PD) of the nipple was first recorded by Sir James Paget in 1874 [1]. Extramammary Paget's disease (EMPD) was not recognized separately until 1889, when it was described by Henry Radcliffe Crocker in ‘Diseases of the skin’ [2].
EMPD is a rare, neoplastic condition. It has been reported to affect any skin or mucosal region but has mainly found on the anogenital regions [3]. A relatively rare condition, it most commonly appears in postmenopausal women of Caucasian heritage, mainly affecting the vulva. The most common symptom is pruritis, and lesions occasionally show hyperpigmentation or hypopigmentation [4]. It has been associated with an underlying in situ or invasive neoplasm in a small proportion of cases (9–32%) in several small studies with an average of 25% dependent on site [4].
EMPD of the oral tissues, an extremely rare condition, was first reported by Changus et al. [5] in 1971. To our knowledge, there are just three globally published cases of EMPD of the oral tissues [5–7].
Here, we present a case of EMPD of the hard palate and a review of the existing literature base.
Case report
A healthy 42-year-old postman presented to his dentist complaining of a 6-month history of itching and discomfort in the maxillary gingivae. After unsuccessful treatment for oral candidiasis, he was provisionally diagnosed with erosive lichen planus and referred to the local maxillofacial department. At initial clinical presentation at the maxillofacial unit, the patient was observed to have florid erythroleukoplakia of the hard palate and buccal gingivae (Fig. 1). All maxillary teeth were found to mobile. There were no cutaneous lesions. A social history revealed a 25-year pack-history of cigarette smoking. The patient admitted to drinking up to eight cans of cider per day.

An incisional biopsy reported that the specimen was consistent with EMPD, with no evidence of invasive malignancy. There were no other differential diagnoses included in the histopathological report. Staging computed tomography scans showed no evidence of invasive disease or distant metastases.
The patient was treated with wide local excision of the mucosa of the hard palate, labial maxillary gingivae and bilateral buccal mucosae. Histopathological analysis of the specimen revealed involvement of all margins with EMPD (Fig. 2).
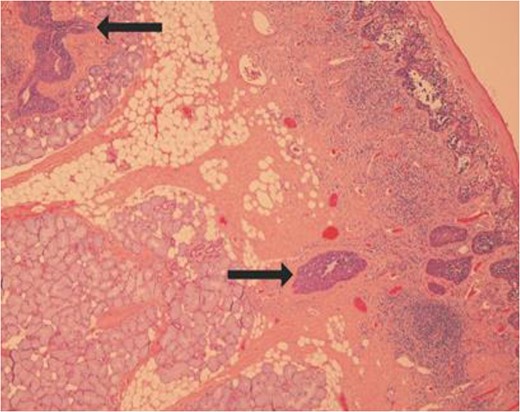
Slide showing ductal colonization by the tumour cells as shown by the arrows.
Following discussion by the head and neck multidisciplinary team, the patient received further wide local excision of the area, dental clearance of the upper arch and reconstruction with a microvascular radial forearm free flap. It was decided that there was no evidence to support the use of either radiotherapy or chemotherapy following surgical treatment.
Discussion
EMPD is a condition that can resemble other causes of inflammatory and infective skin and oral diseases. EMPD is identical in macroscopic and microscopic appearances to mammary PD of the nipple. The distinguishing features between PD and EMPD include the anatomic location, the presence of intracellular mucin and positive staining for glandular cytokeratins and antigens [4].
This case illustrates an exceptionally rare diagnosis. This is a condition that could be misdiagnosed as more commonly seen mucositis conditions such as erosive lichen planus or florid oral candidiasis. The non-specific appearance and clinical features of EMPD may mean that referral for specialist opinion is delayed, and diagnosis may be delayed.
As we have previously noted, there are just three similar cases in the literature to our knowledge. These cases described patients between 50 and 65 years of age; all of whom were at least a decade older than the patient described in this case. All previously described cases featured significant smoking history; and one of significant alcohol consumption also. These cases were all treated with surgical resection and neck dissection of the affected side. The literature does not indicate any methods of reconstruction. In two cases, the patients also received radiotherapy. Both of these patients died <2 years after the initial treatment; one from metastatic lung carcinoma and the other from cerebral haemorrhage, thought to be related to the radiotherapy.
Due to the rarity of this diagnosis and lack of established guidelines for management, this patient will remain under close review. Follow-up schedule and further treatment planning will be developed based on ongoing clinical and radiographic assessment. This case highlights the importance of adding cases of such rarity to the literature in order to facilitate not only evidence-based practice but also patient counselling and education.
Conflict of interest statement
None declared.
Ethics statement/confirmation of patient permission
Ethics statement is not required. The patient has given permission for the case to be reported.



